
Anti-directional cervical intervertebral motion: could it have gone any other way?
The human neck participates in a number of functions, for example, swallowing, breathing and communicating through subtle gestures—and of course, carrying the head as a platform for vision. Seen in its entirety therefore, neck motion may have little reason to be consistent. Yet consistency is what we expect of mechanical systems. If we think of a worn bearing in a car’s water pump, the inconsistent rotation of the pump’s shaft will eventually cause it to fail. However, this illustrates an important difference between these two mechanical systems: the pump has a single function and the cervical linkages have a considerable number of them. The study by Wang et al., in this edition, illustrates this well. By tracking the motion of 7 cervical intervertebral joints from C0 to C7 in healthy, pain-free participants through flexion and extension using fluoroscopy and dividing the motion into 10 epochs, the authors have shown that a considerable proportion of the motion epochs contained anti-directional intervertebral motion. It is difficult to conceive of anything less consistent.
Studies in healthy controls are important, for they provide a baseline for the investigation of patients with painful disorders. They also provide insight into the measurement properties of the variables selected, as well as providing a platform for improvements to the methods for recording and analysis. The authors could have chosen a number of indices to explore; such as IV-RoM, translation and finite centre of rotation. However, these are the legacy of static radiography, which has been used to assess intervertebral displacement (but not strictly motion) for nearly 100 years. These methods are inexpensive and convenient and therefore tend to be preferred to measures that are expensive and complex. However, the current expansion of fluoroscopic video systems that provide individualised, multi-segmental, contemporaneous and automated measurements of intervertebral kinematics is a source of inspiration for many in the spine community. Automated tracking allows the recording and analysis of continuous motion patterns along with new and unfamiliar indices, such as inter segmental laxity and motion apportionment (1,2).
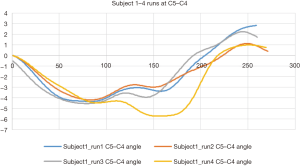
The results of the present study suggest that anti-directional motion is more prevalent in the upper cervical joints. A brief consideration of cervical motion strategies might suggest why this is so. Cervical flexion consists of two motions: nodding and bending—in any order and at any time. Only by strictly standardising these could the neck be constrained to produce the same intervertebral motion patterns in a series of consecutive examinations, especially in the upper cervical spine. Even in the mid-lower cervical spine, an example of four repetitions of the same flexion and return motion (Figure 1) shows apparently related, but different motion patterns at C5–C4, with anti-directional motion occurring during the return phase and ending at a different intervertebral angle. Therefore, in this example, these anti-directional motions were probably compensated at other levels.
Whereas the older literature tended to regard anything that looked ‘odd’ to an ’expert’ as being ‘abnormal’, we have become more critical. A review of the anatomy by Bogduk and Mercer in 2000 concluded that sagittal plane paradoxical (anti-directional) motion of C1 was entirely possible in controls, dependent on the movement strategy adopted by its owner (3). Later, Anderst et al. performed continuous motion analysis with fluoroscopy and found that the initial static position of intervertebral joints and the height of intervertebral discs had greater influence on motion variability than an arthrodesis (4).
Although this was claimed to be the first report of continuous cervical kinematics during in vivo flexion-extension motion, a PhD thesis published by Branney the same year used quantitative fluoroscopy to compare patients receiving manual therapy for subacute and chronic nonspecific neck pain with untreated controls, both at baseline and at 4 weeks follow-up (5). These studies found that patients actually had fewer segments with anti-directional motion than controls. It also examined inter vertebral laxity and found that it too was higher in controls, supporting the hypothesis that a pain-free state is consistent with greater flexibility and thus perhaps greater scope for the variation represented by anti-directional motion. In these studies, despite high measurement reliability, such was the intra-subject variability in controls, that some subjects who did not have anti-directional motion at baseline, developed it at follow-up. Nor did baseline levels of pain, disability or quality of life in patients correlate with its occurrence. This already suggests that anti-directional motion is a natural phenomenon that should not be regarded as a movement pathology.
A further PhD study investigated cervical spine histopathological damage and fractures in people who had suffered fatal whiplash-associated trauma (6). It found surprisingly little of such damage, suggesting that ongoing neck pain in those who survive may have other mechanisms. Subsequently, a role has been suggested for failed intervertebral compensation for day to day stresses in pain generation (7). This could be assessed at intervertebral levels using fluoroscopic video technologies. However, until recently, these have been used almost exclusively for research. This is because studies linking abnormal kinematics to symptoms are lacking, making clinical examinations difficult to justify. Not the least of the work ahead is therefore towards an explanation of the link between kinematics and pain. However, this line of enquiry is fraught with difficult choices, which brings us back to the issue of consistency.
A prominent area of research in spine pain is that of motor control, where symptomatic states are accompanied by impaired proprioception (repositioning studies) and motor control exercises have grown in use as a treatment for low back pain. These attempt to regain consistency in movement behaviour, and could be tested with intervertebral kinematic studies. However, these have yet to show benefits over graded exercises (8). Another theory that could be tested is the relationship between of the locations of finite centres of rotation of cervical vertebrae and the presence of mechanical neck pain (9). Fluoroscopic systems could potentially make this more powerful by providing continuous joint centre analysis as represented by centrode lengths (another reflection of consistency) without high radiation exposure. However, if a spinal motion segment rotates very little, no measurement of a centre of rotation is possible, due to computational error amplification, which is a limitation of this measure (10).
Another option is to avoid explanatory research and investigate treatment effects. Manual therapy and exercises are ideal candidates for this, being recommended in guidelines for the treatment of nonspecific neck pain (11). Here, kinematic measures could become prognostic factors, mediators, moderators or outcome variables—but which ones and which measures of them? The least complex to explore, at least initially, might be prognosis, as it does not assume stability in the kinematic scores over time. If such studies did throw up associations between kinematics and outcome, it would provide a risk-based assessment for chronicity, (but not what to do if such an assessment presaged a poor prognosis).
When considering which mechanical variables to use, the literature does have some advice. That IV-RoM and degree of lordosis have not been seen to change with manual therapy or to be related to outcome, reflects their high variability in healthy populations, making them potentially poor candidates for correlation with symptom severity (12). Translation, while preferred by surgeons when considering stabilisation, would be specific to a subgroup with notably poor restraint, which is probably better assessed by fluoroscopy than by static radiographs. Laxity, a surrogate indicator of the neutral zone is a continuous measure that is accessible with fluoroscopy and has only indirectly been linked to outcomes previously (13). It measures subtle loss of restraint, but needs to be measured passively to avoid the masking effects of muscle guarding. It therefore probably reflects a subgroup.
In the lower back, the apportionment of intervertebral motion between levels across the motion sequence has been found to be more inconsistent in patients with nonspecific back pain and therefore a possible biomarker. This is especially true if there is evidence of additional imposed mechanical disruption of motion segments (such as resected fusion) (14). However, these factors were again only significant during passive recumbent motion, where muscular activity was excluded and motion patterns reflected purely inter vertebral restraint. However, they do implicate pain generating mechanisms that may be worth investigation. This has not yet taken place in the cervical spine.
Possible pain mechanisms in disordered restraint patterns are muscle fatigue, overuse and metabolite accumulations. These parameters may be associated with lack of compensatory kinematics at an intervertebral level and if so, may play a part in nonspecific cervical and lumbar spine pain.
A further factor is the complex interactions between loading, degeneration and sagittal alignment in the cervical spine. We know very little about the relationships between the first two of these and intervertebral kinematics—and the prospect of automated motion analysis of cervical segments that are severely arthritic has yet to be explored. Neck postures and the pathophysiology of fatigue during prolonged static loading tasks are, however, much more ripe for investigation using continuous multilevel assessments, including that of anti-directional motion. Recent studies suggest that it may be possible to amalgamate segmented magnetic resonance imaging (MRI) information in individualised finite element models, with continuous intervertebral motion to predict intersegmental loading during motion (15). This would add a further dimension to intervertebral motion assessment in vivo, by providing individualised stress models—especially if it employed continuous intervertebral motion.
Finally, the desire to explore biological mechanisms in spinal pain should not ignore the effects of the other factors in the biopsychosocial model. Psychosocial factors have been heavily relied on in conservative care over the past few decades and need to be supplemented by validated assessments of the biomechanisms in play (16). Nor can signs of central sensitisation or chemical pain be ignored in patient workups or treatment strategies. Instead, biopsychosocial assessments, expanded when needed by objective and in-depth evaluation of the spine’s ability to compensate for painful mechanical stresses should help to support better-informed treatment choices for patients with these conditions.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Mellor FE, Muggleton JM, Bagust J, et al. Mid-lumbar lateral flexion stability measured in healthy volunteers by in-vivo fluoroscopy. Spine (Phila Pa 1976) 2009;34:E811-7. [Crossref] [PubMed]
- Aiyangar A, Zheng L, Anderst W, et al. Apportionment of lumbar L2-S1 rotation across individual motion segments during a dynamic lifting task. J Biomech 2015;48:3709-15. [Crossref] [PubMed]
- Bogduk N, Mercer S. Biomechanics of the cervical spine. I: Normal kinematics. Clin Biomech (Bristol, Avon) 2000;15:633-48. [Crossref] [PubMed]
- Anderst WJ, Donaldson WF 3rd, Lee JY, et al. Continuous cervical spine kinematics during in vivo dynamic flexion-extension. Spine J 2014;14:1221-7. [Crossref] [PubMed]
- Branney J. An observational study of changes in cervical inter-vertebral motion and the relationship with patient-reported outcomes in patients undergoing spinal manipulative therapy for neck pain. Bournemouth: Bournemouth University, 2014.
- Uhrenholt L. Morphology and pathoanatomy of the cervical spine facet joints in road traffic crash fatalities with emphasis on whiplash – a pathoanatomical and diagnostic imaging study. Available online: http://www.whiplashforskning.dk/articles/PhD-thesis_Uhrenholt_2007.pdf
- Barz T, Melloh M, Lord SJ, et al. A conceptual model of compensation/decompensation in lumbar segmental instability. Med Hypotheses 2014;83:312-6. [Crossref] [PubMed]
- Macedo LG, Latimer J, Maher CG, et al. Effect of Motor Control Exercises Versus Graded Activity in Patients With Chronic Nonspecific Low Back Pain. A Randomized Controlled Trial. Phys Ther 2012;92:363-77. [Crossref] [PubMed]
- Amevo B, Aprill C, Bogduk N. Abnormal instantaneous axes of rotation in patients with neck pain. Spine (Phila Pa 1976) 1992;17:748-56. [Crossref] [PubMed]
- Breen A, Breen A. Accuracy and repeatability of quantitative fluoroscopy for the measurement of sagittal plane translation and finite centre of rotation in the lumbar spine. Med Eng Phys 2016;38:607-14. [Crossref] [PubMed]
- Bussières AE, Stewart G, Al-Zoubi F, et al. The Treatment of Neck Pain-Associated Disorders and Whiplash-Associated Disorders: A Clinical Practice Guideline. J Manipulative Physiol Ther 2016;39:523-64.e27. [Crossref] [PubMed]
- Shilton M, Branney J, de Vries BP, et al. Does cervical lordosis change after spinal manipulation for non-specific neck pain? A prospective cohort study. Chiropr Man Therap 2015;23:33. [Crossref] [PubMed]
- Teyhen DS, Flynn TW, Childs JD, et al. Arthrokinematics in a subgroup of patients likely to benefit from a lumbar stabilization exercise program. Phys Ther 2007;87:313-25. [Crossref] [PubMed]
- Breen A, Mellor F, Breen A. Aberrant intervertebral motion in patients with treatment-resistant nonspecific low back pain: a retrospective cohort study and control comparison. Eur Spine J 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Zanjani-Pour S, Meakin JR, Breen A, et al. Estimation of in vivo inter-vertebral loading during motion using fluoroscopic and magnetic resonance image informed finite element models. J Biomech 2018;70:134-9. [Crossref] [PubMed]
- Deane JA, McGregor AH. Current and future perspectives on lumbar degenerative disc disease: a UK survey exploring specialist multidisciplinary clinical opinion. BMJ Open 2016;6. [Crossref] [PubMed]


