
Length of stay associated with posterior cervical fusion with intervertebral cages: experience from a device registry
Introduction
Spine-related healthcare expenditures have risen dramatically over the past several decades (1). In fact, spinal fusion remains among the costliest operating room procedures performed in the United States (US) (2). Thus, it is imperative to initiate and adopt methods to constrain costs associated with spinal procedures without compromising patient care. Despite technical advances in the diagnosis and treatment of spinal disorders, the length of hospital stay has not improved over time (3). Thus, diminishing length of stay, if accomplished, can be a valuable step in curtailing healthcare expenditures.
When conservative medical management fails to ameliorate chronic symptoms of cervical myeloradiculopathy, operative decompression and fusion is indicated. Although it provides satisfactory clinical results, posterior cervical laminectomy and lateral mass fixation with instrumentation requires wide operative dissection with disruption of musculo-ligamentous and neural structures, resulting in higher blood loss, longer operating time and lengthier hospital stays than anterior fusion approaches (4,5).
An alternative, tissue-sparing posterior fusion procedure has been developed that utilizes a unique set of posterior cervical fusion instruments and intervertebral cages placed posteriorly in the facet joint space to provide indirect neural decompression, stabilization, and promotion of cervical fusion (6,7). Biomechanical investigations of this device have demonstrated similar segmental stability to posterior lateral mass fixation and anterior cervical discectomy and fusion (ACDF) (8,9). Additionally, cadaveric and radiographic studies have confirmed facet distraction with enlargement of foraminal area and width following implantation (10-12). Patients have realized improvements in pain, function and quality of life with this procedure and clinical results have been durable (7,13-15).
The tissue-sparing posterior fusion procedure involves the use of devices that prepare the joint for fusion as well as use of the posteriorly-placed cages. The DTRAX® Spinal System is a set of instruments intended and indicated for access and preparation of a spinal joint to aid in fusion and the CAVUX® cervical cages are indicated for use in skeletally mature patients with degenerative disc disease of the cervical spine with accompanying radicular symptoms. The cages are intended to be used with autogenous bone graft and supplemental fixation. The supplemental fixation may be achieved either with an anterior plating system or ALLY™ bone screw. These products have been available commercially in the US since 2013. A medical device registry was established at several clinical sites in the US to track the ongoing performance and clinical utility of this tissue-sparing spinal fusion approach in a real-world clinical practice setting. Herein, we provide characterization of patients enrolled in the registry with respect to length of stay, estimated blood loss, and procedural time.
Methods
This is a multi-center medical device registry, initiated at 13 clinical sites in the US, to evaluate the ongoing utilization of the CAVUX® cervical cages (Providence Medical Technology, Pleasanton, CA, USA) in the management of symptomatic, degenerative neural compressive disorders of the cervical spine. The primary aim of the registry is to prospectively collect a set of perioperative and clinical outcomes among patients treated with tissue-sparing, posteriorly-placed intervertebral cage fusion.
Characterization and description of the device system, procedural details and surgical technique have been published previously (16). Briefly, using a tissue-sparing posterior approach, the system employs titanium posterior cervical cages that are positioned between the facet joints and supplemented with bone graft to facilitate fusion. The device provides joint distraction and indirect foraminal decompression to alleviate radicular symptoms (11).
The primary aim of this review was to evaluate the data collected relative to the length of hospital stay following posteriorly-placed cervical cage fusion as well as related perioperative characteristics including estimated blood loss and procedural time. Patients were included if they supplied at least one of these three variables and did not undergo any other concomitant procedures in addition to those involving posterior fusion cages at other levels. Under the aegis of the device registry, this study was granted an exemption by an independent central IRB (Ethical and Independent Review Services, Corte Madera, CA, ID #16140-01, #15146-01). All data were de-identified and anonymous, and thus did not require patient informed consent.
Patients were sub-categorized by the type of procedure performed. Three study groups included (I) posteriorly-placed cervical cage fusion as a primary, stand-alone procedure; (II) revision using posteriorly-placed cage fusion for pseudoarthrosis due to non-union after ACDF; and (III) circumferential (360°) fusion consisting of ACDF plus posteriorly-placed cage fusion.
Length of stay data are presented as median and range to assure independence against extreme values. Estimated blood loss and procedural time are shown as mean ± standard deviation. For all variables, data are presented for type of procedure overall and by number of levels treated.
Results
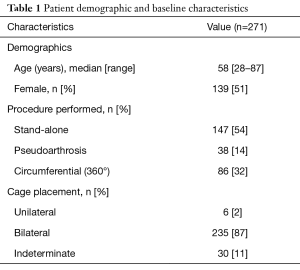
Table 1 provides demographics and background characteristics for 271 patients that were eligible for inclusion in this analysis. In majority of cases (54%), the procedure was performed as a stand-alone intervention and most cases involved the implantation of bilateral, posteriorly-placed cervical cages (87%). Length of stay data were available for 97% (264 of 271) of patients. Estimated blood loss and procedural time were available for 64% (173 of 271) and 62% (167 of 271) of patients, respectively.
Full table
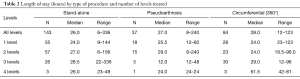
Overall, median length of stay values indicated a brief hospitalization and did not vary notably by type of procedure (range, 26–28 hours). Additionally, length of stay was similarly short and consistent across number of treated levels (Table 2).
Full table
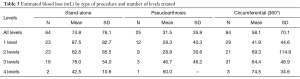
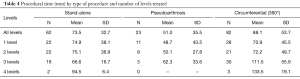
To the contrary, mean estimated blood loss and procedural time values varied widely depending on the type of procedure performed (Tables 3,4). Operative blood loss, however, was extremely low for all patients irrespective of procedure or number of levels treated. Notably, estimated blood loss and corresponding procedural time were uniformly lower in patients undergoing surgery for pseudoarthrosis compared to patients having stand-alone or circumferential procedures. For example, patient undergoing surgery for pseudoarthrosis had less than half the average blood loss as patients having a stand-alone fusion (31.5 vs. 74.8 mL) (Table 3). The mean operative duration was correspondingly lowest among patients having revision surgery for pseudoarthrosis as well (51.0 min) (Table 4). Additionally, procedural time was approximately 20% longer for circumferential fusion compared to stand-alone arthrodesis (88.1 vs. 73.5 min).
Full table
Full table
Discussion
This medical device registry was initiated to capture real world, pragmatic experience regarding the clinical utilization and performance of a novel, cervical cage fusion system for patients with recalcitrant radicular symptoms refractory to conservative management. It expands and compliments other ongoing studies of this device.
We found that tissue-sparing, posteriorly-placed cage fusion was associated with a brief period of hospitalization of approximately 1.2 days irrespective of type of procedure performed or number of levels treated. Commensurately, this procedure also resulted in minimal blood loss and short operative time. Our average length of stay compares favorably with studies employing open posterior lateral mass fixation and instrumented fusion. Numerous single-center studies have reported average lengths of stay following posterior cervical fusion ranging from 4.0 to 7.3 days (3,4,17-22). Several other studies reporting length of stay following posterior cervical fusion are of note due to their large sample sizes. For example, using the Nationwide Inpatient Sample (NIS) from 1,000 randomly selected US hospitals, Shamji et al. (5) reported an average length of stay of 4.1 days in 2,457 posterior cervical fusion procedures. Similarly, in a matched cohort analysis of the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP, 2011–2014) database, 264 patient treated with posterior cervical fusion had a mean length of stay of 4.2 days (23). Finally, Myhre et al. (24) examined the Medicare database and identified 46,171 patients treated with posterior cervical fusion between 2005 and 2012. Their average post-operative length of hospitalization was 6.0 days.
Adding posteriorly-placed cervical cage fusion to ACDF (i.e., circumferential fusion) did not result in increased length of stay among our registry patients. In fact, the median length of stay among this subgroup was 1.2 days which is somewhat shorter than the well-documented average 2-day hospitalization for ACDF patients (5,23,25,26). Based on the findings of this analysis we hypothesize that the major contributor to length of stay is the type of posterior approach performed, open versus tissue-sparing, with the tissue sparing approach having a more favorable length of stay profile.
Our findings for estimated blood loss and procedural time also compare quite favorably with the published literature on posterior lateral mass fixation. Estimated blood loss during an open, posterior cervical fusion range from 225 to 480 mL (4,17-19,22,27), which is substantially greater than our highest average blood loss of 75 mL among stand-alone patients. For procedural time, our highest average estimate in patients having a circumferential fusion, 88 min, was also lower than the range of 110–270 min for posterior cervical fusion (4,17,22,27,28).
Adopting tissue-sparing procedures for treating common degenerative disorders of the lumbar spine has resulted in substantial reductions in length of stay and, correspondingly, in lower costs (29,30). It would seem logical that similar adoption of tissue-sparing, posteriorly-placed cervical cage fusion over the traditional open posterior procedure that involves lateral mass fixation with instrumentation would yield similar cost-constraining benefits. It has been argued that attempts to reduce length of stay do not necessarily translate to lower costs as the bulk of healthcare expenditures takes the form of overhead, or is incurred early in the patients’ hospital stay (31). However, most of the patients treated in this registry required only a single day of hospitalization which is, at minimum, a 3-day reduction in length of stay over posterior lateral mass fixation. Even if only a small percentage of overall costs are incurred during the final hospital day, the difference noted in our comparison remains noteworthy and very likely cost-beneficial.
Conclusions
Patients undergoing posteriorly-placed, cervical cage fusion required brief post-operative hospitalization that was substantially shorter than length of stay associated with open, posterior lateral mass fixation and comparable to ACDF.
Acknowledgements
We thank Terry Meredith for assistance with manuscript preparation. This study was supported by Providence Medical Technology (Pleasanton, CA, USA).
Footnote
Conflicts of Interest: Drs. Siemionow and McCormack have a financial interest in Providence Medical Technology. Drs. Smith, Gillespy, McCormack and Gundanna received remuneration for medical chart review and data collection. Dr. Block received support from Providence Medical Technology to assist in manuscript development.
Ethical Statement: This study was granted an exemption from patient informed consent by an independent central IRB (Ethical and Independent Review Services, Corte Madera, CA, ID #16140-01, #15146-01).
References
- Martin BI, Deyo RA, Mirza SK, et al. Expenditures and health status among adults with back and neck problems. JAMA 2008;299:656-64. [Crossref] [PubMed]
- Weiss AJ, Elixhauser A, Andrews RM. Characteristics of Operating Room Procedures in U.S. Hospitals, 2011: Statistical Brief #170. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD), 2006.
- Marquez-Lara A, Nandyala SV, Fineberg SJ, et al. Current trends in demographics, practice, and in-hospital outcomes in cervical spine surgery: a national database analysis between 2002 and 2011. Spine (Phila Pa 1976) 2014;39:476-81. [Crossref] [PubMed]
- Yuk FJ, Maniya AY, Rasouli JJ, et al. Factors Affecting Length of Stay Following Elective Anterior and Posterior Cervical Spine Surgery. Cureus 2017;9. [PubMed]
- Shamji MF, Cook C, Pietrobon R, et al. Impact of surgical approach on complications and resource utilization of cervical spine fusion: a nationwide perspective to the surgical treatment of diffuse cervical spondylosis. Spine J 2009;9:31-8. [Crossref] [PubMed]
- McCormack BM, Eyster E, Chiu J, et al. Minimally disruptive posterior cervical fusion with DTRAX cervical cage for single level radiculopathy - results in 10 patients at 1-year. Spine Res 2016;2:1-5.
- Smith W, Gillespy M, Huffman J, et al. Anterior Cervical Pseudarthrosis Treated with Bilateral Posterior Cervical Cages. Oper Neurosurg (Hagerstown) 2018;14:236-42. [Crossref] [PubMed]
- Voronov LI, Siemionow KB, Havey RM, et al. Biomechanical evaluation of DTRAX((R)) posterior cervical cage stabilization with and without lateral mass fixation. Med Devices (Auckl) 2016;9:285-90. [Crossref] [PubMed]
- Voronov LI, Siemionow KB, Havey RM, et al. Bilateral posterior cervical cages provide biomechanical stability: assessment of stand-alone and supplemental fixation for anterior cervical discectomy and fusion. Med Devices (Auckl) 2016;9:223-30. [Crossref] [PubMed]
- Leasure JM, Buckley J. Biomechanical evaluation of an interfacet joint decompression and stabilization system. J Biomech Eng 2014.136. [PubMed]
- Siemionow K, Janusz P, Glowka P. Cervical cages placed bilaterally in the facet joints from a posterior approach significantly increase foraminal area. Eur Spine J 2016;25:2279-85. [Crossref] [PubMed]
- Tan LA, Gerard CS, Anderson PA, et al. Effect of machined interfacet allograft spacers on cervical foraminal height and area. J Neurosurg Spine 2014;20:178-82. [Crossref] [PubMed]
- Lenzi J, Nardone A, Passacantilli E, et al. Posterior Cervical Transfacet Fusion with Facetal Spacer for the Treatment of Single-Level Cervical Radiculopathy: A Randomized, Controlled Prospective Study. World Neurosurg 2017;100:7-14. [Crossref] [PubMed]
- Siemionow K, Janusz P, Phillips FM, et al. Clinical and Radiographic Results of Indirect Decompression and Posterior Cervical Fusion for Single-Level Cervical Radiculopathy Using an Expandable Implant with 2-Year Follow-Up. J Neurol Surg A Cent Eur Neurosurg 2016;77:482-8. [Crossref] [PubMed]
- Siemionow K, Monsef JB, Janusz P. Preliminary Analysis of Adjacent Segment Degeneration in Patients Treated with Posterior Cervical Cages: 2-Year Follow-Up. World Neurosurg 2016;89:730.e1-7. [Crossref] [PubMed]
- McCormack BM, Dhawan R. Novel instrumentation and technique for tissue sparing posterior cervical fusion. J Clin Neurosci 2016;34:299-302. [Crossref] [PubMed]
- Carreon L, Glassman SD, Campbell MJ. Treatment of anterior cervical pseudoarthrosis: posterior fusion versus anterior revision. Spine J 2006;6:154-6. [Crossref] [PubMed]
- Elder BD, Sankey EW, Theodros D, et al. Successful anterior fusion following posterior cervical fusion for revision of anterior cervical discectomy and fusion pseudarthrosis. J Clin Neurosci 2016;24:57-62. [Crossref] [PubMed]
- Galhom AE. Multilevel anterior cervical fusion versus posterior cervical laminectomy and lateral mass fixation or laminoplasty for cervical spondylotic myelopathy. Egy Spine J 2015;15:24-36. [Crossref]
- Highsmith JM, Dhall SS, Haid RW Jr, et al. Treatment of cervical stenotic myelopathy: a cost and outcome comparison of laminoplasty versus laminectomy and lateral mass fusion. J Neurosurg Spine 2011;14:619-25. [Crossref] [PubMed]
- Warren DT, Ricart-Hoffiz PA, Andres TM, et al. Retrospective cost analysis of cervical laminectomy and fusion versus cervical laminoplasty in the treatment of cervical spondylotic myelopathy. Int J Spine Surg 2013;7:e72-80. [Crossref] [PubMed]
- Yehya A. The clinical outcome of lateral mass fixation after decompressive laminectomy in cervical spondylotic myelopathy. Alexandria J Med 2015;51:153-9. [Crossref]
- Yue JK, Upadhyayula PS, Deng H, et al. Risk factors for 30-day outcomes in elective anterior versus posterior cervical fusion: A matched cohort analysis. J Craniovertebr Junction Spine 2017;8:222-30. [Crossref] [PubMed]
- Myhre SL, Buser Z, Meisel HJ, et al. Trends and Cost of Posterior Cervical Fusions With and Without Recombinant Human Bone Morphogenetic Protein-2 in the US Medicare Population. Global Spine J 2017;7:334-42. [Crossref] [PubMed]
- Basques BA, Bohl DD, Golinvaux NS, et al. Preoperative factors affecting length of stay after elective anterior cervical discectomy and fusion with and without corpectomy: a multivariate analysis of an academic center cohort. Spine (Phila Pa 1976) 2014;39:939-46. [Crossref] [PubMed]
- Gruskay JA, Fu M, Basques BA, et al. Factors Affecting Length of Stay and Complications After Elective Anterior Cervical Discectomy and Fusion: A Study of 2164 Patients From The American College of Surgeons National Surgical Quality Improvement Project Database (ACS NSQIP). Clin Spine Surg 2016;29:E34-42. [Crossref] [PubMed]
- Yang L, Gu Y, Shi J, et al. Modified plate-only open-door laminoplasty versus laminectomy and fusion for the treatment of cervical stenotic myelopathy. Orthopedics 2013;36:e79-87. [Crossref] [PubMed]
- Fehlings MG, Santaguida C, Tetreault L, et al. Laminectomy and fusion versus laminoplasty for the treatment of degenerative cervical myelopathy: results from the AOSpine North America and International prospective multicenter studies. Spine J 2017;17:102-8. [Crossref] [PubMed]
- Goldstein CL, Macwan K, Sundararajan K, et al. Perioperative outcomes and adverse events of minimally invasive versus open posterior lumbar fusion: meta-analysis and systematic review. J Neurosurg Spine 2016;24:416-27. [Crossref] [PubMed]
- Shields LB, Clark L, Glassman SD, et al. Decreasing hospital length of stay following lumbar fusion utilizing multidisciplinary committee meetings involving surgeons and other caretakers. Surg Neurol Int 2017;8:5. [Crossref] [PubMed]
- Taheri PA, Butz DA, Greenfield LJ. Length of stay has minimal impact on the cost of hospital admission. J Am Coll Surg 2000;191:123-30. [Crossref] [PubMed]


