
The K-line in the cervical ossification of the posterior longitudinal ligament is different on plain radiographs and CT images
Introduction
Laminoplasty (LMP) is a widely accepted surgical procedure for treating cervical ossification of the longitudinal ligament (OPLL) (1,2). The rationale of LMP is indirect decompression from anterior compressive factors via a “bow-stringing effect” based on lordotic cervical spine curvature (3). LMP in cases of OPLL with significant cervical kyphosis and/or thick ossification often deteriorates into unfavorable results because the bow-stringing effect after LMP is not effective in such patients (4-6). Therefore, LMP should be avoided in patients with significant preoperative kyphosis and/or OPLL with spinal canal compromise of more than 50–60% (7-12).
The “K-line”, which is a virtual line between the midpoints of the anteroposterior canal diameter at C2 and C7, is a useful prognostic indicator for sufficient decompression by LMP for OPLL with kyphosis and/or thick ossification foci. The K-line can reflect both the alignment and the thickness of the OPLL, which determine the surgical outcomes (13,14).
Originally, the K-line is measured with a plain cervical spine lateral radiograph obtained while the patient is in a standing position. However, several surgeons measure the K-line with sagittal reconstruction computed tomography (CT) multiplanar reconstruction (MPR) images, which can clearly reveal the precise size and morphology of the ossification foci (15,16). However, alteration in alignment of the cervical spine between a standing lateral radiograph and CT obtained while the patient is in a supine position, may potentially influence the K-line determination.
The purpose of the present study was to analyze whether there is a difference in K-lines obtained from radiographs of standing patients and those obtained from CT-MPR images of supine patients.
Methods
The present study included 65 patients with cervical OPLL who underwent surgical treatment in our institution from January 2008 through May 2015. The male to female ratio was 10:3, and the mean age of the patients was 63.0 years (range, 36–83 years). The study population consisted of patients with different types of OPLL according to its classification by lateral plain radiographs (17): mixed (n=39), segmental (n=23), continuous (n=2), and circumscribed (n=1).
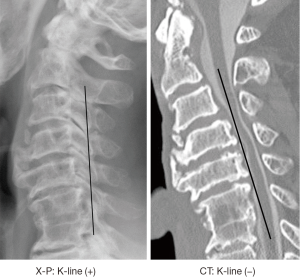
All imaging was performed preoperatively. The K-line was drawn as a virtual line between the midpoints of the anteroposterior canal diameter at C2 and C7 in both plain lateral cervical spine radiographs taken in standing patients in a neutral position (X-P-based K-line) and CT-MPR midsagittal images obtained in supine patients (CT-based K-line). The K-line was defined as (+) when the OPLL peak did not exceed the K-line and (–) when the OPLL peak exceeded the K-line (13). The C2–C7 angle, which is an indicator of cervical alignment, was measured as the angle between the inferior endplates of C2 and C7 vertebrae. The C2–C7 angle was measured from plain lateral cervical spine radiographs of standing patients in a neutral position and CT-MPR midsagittal images. The X-P-based and CT-based K-lines were compared and differences between them were assessed. The differences between C2–C7 angles obtained from plain radiographs and CT-MPR were also assessed.
Results
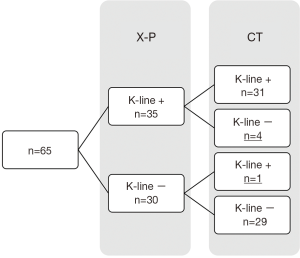
The X-P-based K-line was found to be (+) in 35 patients and (–) in 30 patients, whereas the CT-based K-line was found to be (+) in 32 patients and (–) in 33 patients. Therefore, four of 35 patients with an X-P-based K-line (+) (11%) showed a change from K-line (+) to K-line (–) in CT-based K-line measurement, whereas 31 of 35 patients with an X-P-based K-line (+) (89%) did not show changes in the K-line between X-P-based and CT-based measurements. One of 30 patients with an X-P-based K-line (–) (3%) showed a change from (–) to (+) in CT-based measurements, whereas 29 patients with an X-P-based K-line (–) (97%) did not show any change in the K-line between X-P-based and CT-based measurements (Figures 1,2).
The average C2–C7 angle measured with plain lateral radiographs in standing patients was 6.4°±9.0°, whereas the average C2–C7 angle measured with CT-MPR images in supine patients was 3.6°±20.3°. There was a significant difference between the C2–C7 angle obtained between the two methods of measurement (P=0.012). Where patients showed a change of K-line between the two methods, the C2–C7 angle changed. The average C2–C7 angle in four patients who showed change from a X-P-based K-line (+) to a CT-based K-line (–) changed from 9.3° to –9.5°, showing 18.8° decrease. The average C2–C7 angle in patients who showed a change from a X-P-based K-line (–) to a CT-based K-line (+) changed from –13.5° and –4.8°, showing 8.7° increase. Where the K-line was not altered between the methods of measurement, there was no significant difference in the average C2–C7 angle obtained by the different methods. The average C2–C7 angle in patients with a K-line (+) that did not change between the methods of measurement was 11.1° in radiographs and 11.2° in CT-MPR images. The average C2–C7 angle in patients with a K-line (–) that did not change between the methods of measurement was 1.6° in radiographs and –2.3° in CT-MPR images.
Discussion
The present results showed that the K-line could be different according to the imaging method used to measure it because of a difference in spinal alignment between the methods of measurement.
The K-line can reflect theoretically two different factors important for spinal cord compression, cervical alignment and the thickness of the ossification foci (13). Therefore, the difference in the C2–C7 angle is the sole reason for a difference in K-line found when it is measured from plain radiographs in standing patients or CT-MPR images from supine patients.
Possible reasons for the difference in C2–C7 angle found between plain radiographs of standing patients and CT-MPR images from supine patients, which results in a difference in the K-line, are as follows. First, change of thoracic spine alignment between the standing and supine position can influence the cervical alignment. There is a significant sequential relationship between C2–C7 angle and T1 slope (18). The mean T1 slope in the supine position is less than that in the standing position because of the effect of gravity (19), resulting in a decrease of C2–C7 angle as measured in CT images from supine patients. Next, relative flexion of the neck might result when examiners or the patients themselves attempt to avoid aggravating spinal cord compression. In most patients with cervical OPLL, spinal cord compression can increase and myelopathy can become worse during neck extension (20). Radiographers generally avoid neck extension during CT examinations to avoid aggravating myelopathy symptoms. Similarly, patients themselves might avoid neck extension as an escape reaction. Third, a shoulder hump can affect the thoracic and cervical alignment in the supine position especially in obese patients.
Because the K-line can predict sufficient decompression by LMP, we determine surgical approaches for OPLL patients based on the preoperative K-line. We apply LMP for patients with a K-line (+), whereas we apply anterior decompression and fusion (ADF), or posterior decompression with instrumented fusion (PDF), for patients with a K-line (–) (14) because LMP often deteriorates into unfavorable neurological recovery as a result of insufficient decompression for patients with a K-line (–). Therefore, there is a possibility that alteration of the K-line can affect the choice of surgical approaches to cervical OPLL. CT-based K-line measurements might result in over indication of ADF or PDF, instead of appropriate LMP, because the K-line can change from (+) to (–) when measured from CT-MPR images. In the present series, four patients showed a change from an X-P-based K-line (+) to a CT-based K-line (–) and underwent ADF or PDF instead of LMP. These patients could have been treated more appropriately by LMP. Although the postoperative course of these patients was uneventful, decisions regarding surgical procedures for treatment of cervical OPLL may be adversely influenced by a K-line determined from CT-MPR images. The procedure chosen may be different to the procedure that would have been chosen based on a K-line determined from a radiograph of a patient standing in a neutral position.
When it is difficult to measure the K-line radiographically because of limitations imposed by the anatomical interference of the shoulder contour, which occurs most commonly in obese patients, it is important to be careful when evaluating the K-line obtained from CT-MPR images of supine patients because the K-line can be different to an X-P-based K-line obtained from radiographs of standing patients.
Conclusions
Spinal surgeons should be aware that the K-line obtained from plain radiographs of standing patients and that obtained from CT-MPR images of patients in a supine position may be different. X-P-based K-lines are strongly recommended for surgical decision making.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethical Committee review was waived for this retrospective analysis of radiographs and CT images. Informed written consent was obtained from all patients.
References
- Matsumoto M, Chiba K, Toyama Y. Surgical Treatment of Ossification of the Posterior Longitudinal Ligament and Its Outcomes. Spine 2012;37:E303-8. [Crossref] [PubMed]
- Hirabayashi K, Toyama Y, Chiba K. Expansive laminoplasty for myelopathy in ossification of the longitudinal ligament. Clin Orthop 1999.35-48. [Crossref] [PubMed]
- Aita I, Hayashi K, Wadano Y, et al. Posterior movement and enlargement of the spinal cord after cervical laminoplasty. J Bone Joint Surg Br 1998;80:33-7. [Crossref] [PubMed]
- Chiba K, Ogawa Y, Nakamura M, et al. Long-term results of expansive open-door laminoplasty for cervical myelopathy--average 14-year follow-up study. Spine 2006;31:2998-3005. [Crossref] [PubMed]
- Iwasaki M, Okuda S, Miyauchi A, et al. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: Part 1: Clinical results and limitations of laminoplasty. Spine 2007;32:647-53. [Crossref] [PubMed]
- Yamazaki A, Homma T, Uchiyama S, et al. Morphologic limitations of posterior decompression by midsagittal splitting method for myelopathy caused by ossification of the posterior longitudinal ligament in the cervical spine. Spine 1999;24:32-4. [Crossref] [PubMed]
- Tani T, Ushida T, Ishida K, et al. Relative safety of anterior microsurgical decompression versus laminoplasty for cervical myelopathy with a massive ossified posterior longitudinal ligament. Spine 2002;27:2491-8. [Crossref] [PubMed]
- Iwasaki M, Okuda S, Miyauchi A, et al. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: Part 2: Clinical results and limitations of laminoplasty. Spine 2007;32:654-60. [Crossref] [PubMed]
- Sakai K, Okawa A, Takahashi M, et al. Five-year follow-up evaluation of surgical treatment for cervical myelopathy caused by ossification of the posterior longitudinal ligament: a prospective comparative study of anterior decompression and fusion with floating method versus laminoplasty. Spine 2012;37:367-76. [Crossref] [PubMed]
- Fujimori T, Iwasaki M, Okuda S, et al. Long-term results of cervical myelopathy due to ossification of the posterior longitudinal ligament with an occupying ratio of 60% or more. Spine 2014;39:58-67. [Crossref] [PubMed]
- Houten JK, Cooper PR. Laminectomy and posterior cervical plating for multilevel cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament: effects on cervical alignment, spinal cord compression, and neurological outcome. Neurosurgery 2003;52:1081-7. [PubMed]
- Matsumoto M, Chiba K, Toyama Y. Surgical treatment of ossification of the posterior longitudinal ligament and its outcomes: posterior surgery by laminoplasty. Spine 2012;37:E303-8. [Crossref] [PubMed]
- Fujiyoshi T, Yamazaki M, Koda M, et al. A new concept for making decisions regarding the surgical approach for cervical ossification of the posterior longitudinal ligament: the K-line. Spine 2008;33:E990-3. [Crossref] [PubMed]
- Koda M, Mochizuki M, Konishi H, et al. Comparison of clinical outcomes between laminoplasty, posterior decompression with instrumented fusion, and anterior decompression with fusion for K-line (-) cervical ossification of the posterior longitudinal ligament. Eur Spine J 2016;25:2294-301. [Crossref] [PubMed]
- Kawaguchi Y, Matsumoto M, Iwasaki M, et al. New classification system for ossification of the posterior longitudinal ligament using CT images. J Orthop Sci 2014;19:530-6. [Crossref] [PubMed]
- Smith ZA, Buchanan CC, Raphael D, et al. Ossification of the posterior longitudinal ligament: pathogenesis, management, and current surgical approaches. A review. Neurosurg Focus 2011;30. [Crossref] [PubMed]
- The ossification of the posterior longitudinal ligament of the spine (OPLL). The Investigation Committee on OPLL of the Japanese Ministry of Public Health and Welfare. Nihon Seikeigeka Gakkai Zasshi 1981;55:425-40. [PubMed]
- Lee SH, Son ES, Seo EM, et al. Factors determining cervical spine sagittal balance in asymptomatic adults: correlation with spinopelvic balance and thoracic inlet alignment. Spine J 2015;15:705-12. [Crossref] [PubMed]
- Jun HS, Chang IB, Song JH, et al. Is it possible to evaluate the parameters of cervical sagittal alignment on cervical computed tomographic scans? Spine 2014;39:E630-6. [Crossref] [PubMed]
- Yoshii T, Yamada T, Hirai T, et al. Dynamic changes in spinal cord compression by cervical ossification of the posterior longitudinal ligament evaluated by kinematic computed tomography myelography. Spine 2014;39:113-9. [Crossref] [PubMed]


