
Evaluating cervical deformity corrective surgery outcomes at 1-year using current patient-derived and functional measures: are they adequate?
Introduction
Cervical deformity (CD) is becoming increasingly recognized and effective surgical correction has received much attention recently (1-5). Classifications of CD are not yet fully established and treatment options and surgical correction are dependent on the specific nature of the condition. Assessment of cervical deformities is challenging, given the heterogenic nature of the condition and varying surgical strategies. The primary goals of CD treatment are to restore cervical sagittal alignment and improve horizontal gaze, decompress the neural elements, improve neck pain and overall functional outcomes.
The effects of surgical correction of CD on patient outcomes are not well-defined. Some studies have shown that the concomitant presence CD results in worse clinical outcomes for patients undergoing surgical correction of adult thoraco-lumbar deformity, though further work is warranted to assess extended follow-up for these patients (6,7). It has also been shown that a greater degree of deformity correction correlates with improvements in HRQLs and increased patient satisfaction following CD surgical correction (4,8-10). Tang et al. (10) found that positive sagittal malalignment in the cervical spine, using C2–C7 SVA, negatively impacts SF-36 physical component scores and positively correlates with NDI at early follow-up for multilevel posterior cervical fusions for stenosis, myelopathy, and kyphosis patients.
The current HRQL metrics used to assess patient outcomes following surgical correction of CD are not specific to a CD population. The modified Japanese Orthopaedic Association (mJOA) questionnaire has been validated for cervical myelopathy patients. The neck disability index (NDI) has been validated for cervical radiculopathy, unspecified neck pain, and mechanical neck disorders (11-14). Most recently, Carreon et al. used the NDI to assess cervical degenerative patients’ outcomes following cervical fusions (15). EuroQol five-dimensions (EQ-5D) questionnaire has been used to assess overall health state of patients, but is not specific to CD patients (16).
The present study aims to evaluate the sensitivity of various health-related quality of life (HRQL) outcome measures in assessing CD patients’ outcomes at 1-year post-operatively, in light of the fact that no current HRQL measure is CD specific.
Methods
Data source
This study is a retrospective review of a prospectively-collected database of adult CD patients enrolled from 13 sites around the U.S. Internal Review Board approval was obtained at each participating site prior to study initiation. Inclusion criteria for the database were patients ages ≥18 years, and radiographic evidence of CD at baseline assessment, defined as the presence of at least 1 of the following: cervical kyphosis (C2–7 Cobb angle >10°), cervical scoliosis (C2–7 coronal Cobb angle >10°), C2–7 sagittal vertical axis (cSVA) >4 cm, or chin-brow vertical angle (CBVA) >25°. Patients with active tumors or infections were excluded from the study.
Data collection
Demographic and clinical data collected included patient age, sex, body mass index (BMI), history of prior cervical surgery, baseline mJOA score and baseline T4–T12 thoracic kyphosis. Surgical data collected included operative time, estimated blood loss, surgical approach, bone morphogenetic protein 2 (BMP-2) use, osteotomy use and number of osteotomies, levels fused, and instrumentation used.
Patients were evaluated using full-length free-standing lateral spine radiographs (36’ cassette) at baseline and 1-year post-operative follow-up visit. Radiographs were analyzed using dedicated and validated software (SpineView®; ENSAM, Laboratory of Biomechanics, Paris, France) at a single center with standard techniques (17-19). Measured cervical spine parameters (Figure 1) included cervical SVA (cSVA: offset from the C2 plumbline and the postero-superior corner of C7), C2–C7 lordosis (CL: Cobb angle between C2 inferior endplate and C7 inferior endplate), T1 slope minus CL (TS-CL: mismatch between T1 slope and cervical lordosis), and CBVA (angle subtended between the vertical line and the line from the brow to the chin). Spinopelvic parameters (Figure 1) included: SVA (C7 plumb line relative to the posterosuperior corner of S1), pelvic incidence minus lumbar lordosis (PI-LL: mismatch between pelvic incidence and lumbar lordosis), and pelvic tilt (PT: angle between the vertical and the line through the sacral midpoint to the center of the two femoral heads).
Clinical outcomes assessment
Clinical outcomes were assessed using mJOA, NDI and EQ-5D scores at baseline and 1-year following surgery. The minimum clinically important difference (MCID) for the mJOA was set at 2 based on published values (20). The MCID for NDI was set as 15 (we doubled the published MCID value because our NDI is on a 0–100 scale) and the EQ5D MCID was recently set as 0.1 based on previously published values (15,21,22).
Statistical analysis
Descriptive statistics were first used to summarize the characteristics of the population. Proportions were used to summarize categorical variables and mean ± standard deviation for continuous variables.
To assess the sensitivity of mJOA and NDI in capturing outcomes for a CD population, five anchoring groups were created based on self-reported EQ5D scores: ‘much better’ was assigned to patients to reached the 1-year MCID in EQ5D, ‘better’ for patients who improved in EQ5D though did not reach MCID, ‘neither’ was assigned to patients whose EQ5D scores were the same at baseline and 1-year, ‘worse’ for patients who worsened in EQ5D from baseline to 1-year by 0.5 or less, and ‘much worse’ for patients who worsened in EQ5D by greater than 0.5. mJOA and NDI scores at baseline, 1-year post-operatively, and the change from baseline to 1-year in each metric were assessed among anchor groups. ANOVA with Bonferroni post-hoc analysis was used to assess outcomes based on mJOA and NDI scores among the anchoring groups.
Results are reported as coefficient with SD or odds ratios with 95% confidence intervals with P value. Two-sided P values <0.05 were considered to be statistically significant. All statistical analysis was conducted in SPSS version 23.
Results
Patient population
Sixty-three adult CD patients were included in the analysis. The mean age was 62.52±10.66 years old, mean BMI was 28.58±8.07 kg/m2, average CCI was 0.54±0.89, and 55.6% were female. Twenty-three (37.7%) patients had a history of prior cervical spine surgery; 18 (30.5%) have a history of smoking, 7 (11.1%) have diabetes, 9 (14.3%) have osteoporosis, and 16 (25.4%) have depression. The average baseline NDI score was 46.75, mJOA score was 13.68, and EQ-5D was 0.74. The overall myelopathy score category breakdown at baseline: 9.5% none, 30.2% mild, 42.9% moderate, 17.5% high.
The average levels fused was 7.52±3.56 levels. The average estimated blood loos was 771.60±882.70 mL and the average operative time was 279.28±159.17 minutes. By surgical approach, 31 (49.2%) of surgeries were posterior-only, 11 (17.5%) were anterior-only, and 21 (33.3%) were combined approach. 41.3% of surgeries used BMP-2. Fifteen (23.8%) of patients had a Smith-Peterson osteotomy and 14 (22.2%) had a three-column osteotomy.
Radiographic improvement
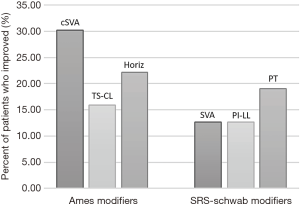
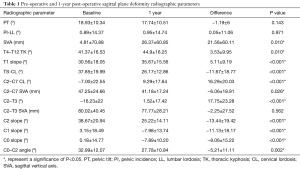
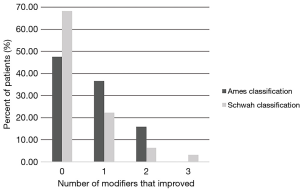
The average baseline cSVA was 47.25±24.66 mm, TS-CL was 37.85°±19.99°, and global SVA was 4.81±70.88 mm (Table 1). Patients significantly improved in SVA, TK, T1 slope, CL, cSVA, C2–T3, C2 slope, C1 slope, C0 slope, and C0–C2 angle from baseline to 1-year post-operatively (all P<0.05). Using the Ames classification for CD, 30.2% of patients improved in cSVA modifier grade from baseline to 1-year post-operative, 15.9% improved in TS-CL modifier grade, and 22.2% in the horizontal gaze modifier grade (Figure 1). Using the SRS-Schwab classification, 12.7% improved in SVA modifier grade, 12.7% in PI-LL grade, and 19.0% in PT grade. Overall, 52.3% of patients improved in at least one Ames modifier and 31.7% of patients improved in at least one SRS-Schwab modifier at 1-year (Figure 2).
Full table
Clinical improvement
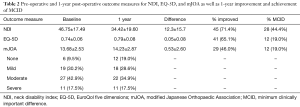
At 1 y, 46.0% of patients improved in mJOA, 71.4% in NDI scores, and 65.1% improved in EQ5D (Table 2); 19.0% of patients met mJOA MCID, 44.4% met NDI MCID, and 19.0% met EQ5D MCID at 1 y. For patients who improved in mJOA at 1 y, baseline mJOA scores were 30.2% mild, 42.9% moderate, and 17.5% severe myelopathy.
Full table
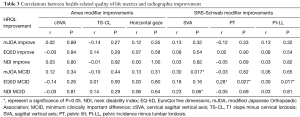
Correlations between HRQL and radiographic improvement
When looking at the correlations between radiographic and HRQL improvement, there was no correlation between improvement in Ames radiographic modifier grades and HRQL improvement in the overall cohort (Table 3). Improvement in Schwab SVA modifier grade correlated with reaching 1-year mJOA MCID (r=0.30, P=0.017). Both Schwab PT and PI-LL modifier grade improvements were correlated with reaching 1-year EQ-5D MCID (r=0.28, P=0.027; r=0.30, P=0.017). In looking only at patients without severe concomitant thoracolumbar malalignment, improvement in the Ames horizontal gaze modifier grade approached significant correlation with reaching 1-year mJOA MCID (r=0.27, P=0.051).
Full table
Multivariate analysis
A one-point improvement in NDI score increased the odds of improving in mJOA and reaching 1 y mJOA MCID (mJOA improvement: OR, 1.06, CI: 1.01–1.10, P=0.01; mJOA MCID: OR, 1.06, CI: 1.02–1.11, P=0.006). Improvement in EQ-5D by 0.1 increased the odds of improving in mJOA and of reaching mJOA MCID at 1 y (improvement: OR, 3.85, CI: 1.51–9.76, P=0.005; MCID: OR, 3.88, CI: 1.52–9.88, P=0.005). Reaching 1 y mJOA MCID was correlated with EQ-5D score improvement (EQ-5D: r=0.355, P=0.004). While correlations were seen between outcome measures, when modeling these outcomes while controlling for confounders including cSVA change, surgical invasiveness, age and CCI, these HRQLs were not strongly correlated.
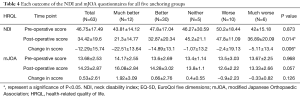
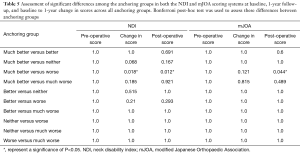
Anchoring groups and comparison of outcomes for mJOA and NDI
The breakdown of the anchoring groups was as follows: 12 patients (19%) were in the ‘much better’ group, 30 patients (47.6%) in the ‘better’ group, 5 patients (7.9%) in the ‘neither’ group, 10 patients (15.9%) in the ‘worse’ group, and 6 patients (9.5%) in the ‘much worse’ group (Table 4). One-year NDI score (P=0.014) and baseline to 1-year change in NDI score (P=0.006) were different across anchoring groups (Table 5). Baseline to 1-year change in NDI scores were significantly different between the ‘much better’ and ‘worse’ groups (‘much better’ Δ=−22.0 points, ‘worse’ Δ=−2.4 points, P=0.018). One-year NDI scores (‘much better’ =21.0, ‘worse’ =47.0, P=0.012) and 1-year mJOA scores (‘much better’ =16.08, ‘worse’ =12.60, P=0.044) were also different between those same two groups All other anchoring groups did not display significant differences in mJOA or NDI scores (all P>0.1).
Full table
Full table
Discussion
With the lack of a CD-specific patient outcomes measurement, the need arises to assess the current outcome metrics in the context of CD to evaluate their effectiveness. Improvements in NDI and EQ-5D increased the likelihood of improving or reaching MCID for mJOA. However, these direct relationships between mJOA, NDI, and EQ-5D were not maintained in an adjusted model controlling for confounding factors, possibly because these outcome measures assess different aspects of a patient’s disability, and they are also not specific to a CD population. Outcomes following corrective surgery for CD are not as profound or clear as compared to adult spinal deformity results. There has been little work done to evaluate outcomes following surgical correction specifically for a CD population. Theologis et al. found that patients with cervicothoracic junction deformities had improved quality of life after three column posterior osteotomies (23). Another group reported NDI improvements following pedicle subtraction osteotomy at the cervicothoracic junction for cervical sagittal imbalance (3). In addition, studies have shown that patients with CD and concomitant thoracolumbar deformity have improved outcomes following corrective surgery (6,7,24). We found that at 1-year post-operatively, 46% of patients improved in mJOA, 71.4% in NDI, and 65.1% in EQ-5D, with a subset of patients reaching MCID improvements in each outcome measure.
When looking at the correlations between improvements in radiographic measures and HRQL measures, we found no significant relationships between improvements in Ames radiographic modifiers and improvements in mJOA, NDI, or EQ-5D. However, some improvements in SRS-Schwab modifiers (PT and PI-LL) were correlated with reaching the MCID for EQ-5D and SVA improvements were correlated with MCID for mJOA and NDI. There have been few studies to report the relationships between radiographic parameters in the cervical spine, specific to a deformity population, and HRQL measures (10,25). These relationships are not as well-established as the global and pelvic parameters’ relationships with outcomes for thoracolumbar deformity (26-28). Of the few studies looking into these relationships for cervical patients, one found no significant relationships between segmental kyphosis and post-operative outcomes and another concluded that only segmental sagittal alignment correlated with clinical outcomes after cervical disc arthroplasty but overall cervical alignment did not correlate with outcomes (25,29,30). In addition, we found, using EQ-5D as an anchor, that patients who were ‘much better’ had significantly lower NDI scores and higher mJOA scores at 1-year follow-up than patients who were ‘worse’.
This study is one of the first to investigate clinical outcomes following CD corrective surgery. We found that improving by one-point on the NDI or EQ-5D questionnaires increased the odds of improving in mJOA score and reaching the MCID for mJOA. However, no significant correlations were seen between radiographic parameters and improvements and HRQLs. This might be attributable to the use of current metrics that are not specific enough for CD or because we are weighting radiographic parameters too heavily, or possibly a combination of these two. Similarly, a recent study found that when looking at lumbar lordosis index and global tilt, only 2% of the variance in ODI was attributable to radiographic parameters (31). When modeling these outcomes, controlling for many confounding factors, we found that these HRQLs were not strongly correlated. Given that none of these outcome measures are specific for assessing CD, a strong correlation between outcome measures that assess various aspects of a patient’s disability and health state might not be achievable.
Limitations
We appreciate several limitations. Firstly, the retrospective, multicenter nature of this study creates the possibility for surgeon and site variation, though the benefits of a multicenter study are that it allows for more generalizability to the findings. With relatively short follow-up, this study should be re-evaluated using longer follow-up to fully assess the relationship between these metrics in a CD population.
Conclusions
This study found that improvements in mJOA score were correlated with changes in NDI and EQ-5D. Using an adjusted model that took into account many factors including change in cSVA, invasiveness, CCI, and age, the direct relationships between these patient outcome measures were not maintained. Since these patient-reported outcomes do not strongly correlate with each other or with radiographic parameters, perhaps a metric that more strongly correlates with relevant radiographic and clinical outcome metrics specific to a CD population is necessary. Further studies with an increased number of patients and longer follow-up are required to fully assess these relationships between outcome measures and radiographic parameters as well as to work towards the development of a cervical-deformity specific outcome metric.
Acknowledgements
The International Spine Study Group (ISSG) is funded through research grants from DePuy Synthes and individual donations.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by their local Institutional Review Board (No. 12-02939) and written informed consent was obtained from all patients.
References
- Smith JS, Klineberg E, Shaffrey CI, et al. Assessment of Surgical Treatment Strategies for Moderate to Severe Cervical Spinal Deformity Reveals Marked Variation in Approaches, Osteotomies, and Fusion Levels. World Neurosurg 2016;91:228-37. [Crossref] [PubMed]
- Nottmeier EW, Deen HG, Patel N, et al. Cervical kyphotic deformity correction using 360-degree reconstruction. J Spinal Disord Tech 2009;22:385-91. [Crossref] [PubMed]
- Deviren V, Scheer JK, Ames CP. Technique of cervicothoracic junction pedicle subtraction osteotomy for cervical sagittal imbalance: report of 11 cases. J Neurosurg Spine 2011;15:174-81. [Crossref] [PubMed]
- Grosso MJ, Hwang R, Mroz T, et al. Relationship between degree of focal kyphosis correction and neurological outcomes for patients undergoing cervical deformity correction surgery. J Neurosurg Spine 2013;18:537-44. [Crossref] [PubMed]
- Han K, Lu C, Li J, et al. Surgical treatment of cervical kyphosis. Eur Spine J 2011;20:523-36. [Crossref] [PubMed]
- Protopsaltis TS, Scheer JK, Terran JS, et al. How the neck affects the back: changes in regional cervical sagittal alignment correlate to HRQOL improvement in adult thoracolumbar deformity patients at 2-year follow-up. J Neurosurg Spine 2015;23:153-8. [Crossref] [PubMed]
- Passias PG, Soroceanu A, Smith J, et al. Postoperative cervical deformity in 215 thoracolumbar patients with adult spinal deformity: prevalence, risk factors, and impact on patient-reported outcome and satisfaction at 2-year follow-up. Spine (Phila Pa 1976) 2015;40:283-91. [Crossref] [PubMed]
- Etame AB, Wang AC, Than KD, et al. Outcomes after surgery for cervical spine deformity: review of the literature. Neurosurg Focus 2010;28. [Crossref] [PubMed]
- Villavicencio AT, Babuska JM, Ashton A, et al. Prospective, randomized, double-blind clinical study evaluating the correlation of clinical outcomes and cervical sagittal alignment. Neurosurgery 2011;68:1309-16. [Crossref] [PubMed]
- Tang JA, Scheer JK, Smith JS, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery 2012;71:662-9; discussion 669. [Crossref] [PubMed]
- Jorritsma W, Dijkstra PU, de Vries GE, et al. Detecting relevant changes and responsiveness of Neck Pain and Disability Scale and Neck Disability Index. Eur Spine J 2012;21:2550-7. [Crossref] [PubMed]
- Pool JJ, Ostelo RW, Hoving JL, et al. Minimal clinically important change of the Neck Disability Index and the Numerical Rating Scale for patients with neck pain. Spine (Phila Pa 1976) 2007;32:3047-51. [Crossref] [PubMed]
- Cleland J a. Childs JD, Whitman JM. Psychometric Properties of the Neck Disability Index and Numeric Pain Rating Scale in Patients With Mechanical Neck Pain. Arch Phys Med Rehabil 2008;89:69-74. [Crossref] [PubMed]
- Young IA, Cleland JA, Michener LA, et al. Reliability, construct validity, and responsiveness of the neck disability index, patient-specific functional scale, and numeric pain rating scale in patients with cervical radiculopathy. Am J Phys Med Rehabil 2010;89:831-9. [Crossref] [PubMed]
- Carreon LY, Glassman SD, Campbell MJ, et al. Neck Disability Index, short form-36 physical component summary, and pain scales for neck and arm pain: the minimum clinically important difference and substantial clinical benefit after cervical spine fusion. Spine J 2010;10:469-74. [Crossref] [PubMed]
- Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med 2001;33:337-43. [Crossref] [PubMed]
- Champain S, Benchikh K, Nogier A, et al. Validation of new clinical quantitative analysis software applicable in spine orthopaedic studies. Eur Spine J 2006;15:982-91. [Crossref] [PubMed]
- Rillardon L, Levassor N, Guigui P, et al. Validation of a tool to measure pelvic and spinal parameters of sagittal balance. Rev Chir Orthop Reparatrice Appar Mot 2003;89:218-27. [PubMed]
- O’Brien MF, Kuklo TR, Blanke KM, et al. Spinal Deformity Study Group Radiographic Measurement Manual. Memphis, TN: Medtronic Sofamor Danek, 2005.
- Tetreault L, Kopjar B, Arnold P, et al. A Clinical Prediction Rule for Functional Outcomes. J Bone Joint Surg Am 2015;97:2038-46. [Crossref] [PubMed]
- Le QA, Doctor JN, Zoellner LA, et al. Minimal clinically important differences for the EQ-5D and QWB-SA in Post-traumatic Stress Disorder (PTSD): results from a Doubly Randomized Preference Trial (DRPT). Health Qual Life Outcomes 2013;11:59. [Crossref] [PubMed]
- Parker SL, Adogwa O, Paul AR, et al. Utility of minimum clinically important difference in assessing pain, disability, and health state after transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Neurosurg Spine 2011;14:598-604. [Crossref] [PubMed]
- Theologis AA, Tabaraee E, Funao H, et al. Three-column osteotomies of the lower cervical and upper thoracic spine: comparison of early outcomes, radiographic parameters, and peri-operative complications in 48 patients. Eur Spine J 2015;24 Suppl 1:S23-30. [Crossref] [PubMed]
- Scheer JK, Passias PG, Sorocean AM, et al. Association between preoperative cervical sagittal deformity and inferior outcomes at 2-year follow-up in patients with adult thoracolumbar deformity: analysis of 182 patients. J Neurosurg Spine 2016;24:108-15. [Crossref] [PubMed]
- Scheer JK, Tang JA, Smith JS, et al. Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine 2013;19:141-59. [Crossref] [PubMed]
- Schwab FJ, Smith VA, Biserni M, et al. Adult scoliosis: a quantitative radiographic and clinical analysis. Spine (Phila Pa 1976) 2002;27:387-92. [Crossref] [PubMed]
- Schwab FJ, Farcy J, Bridwell K, et al. A clinical impact classification of scoliosis in the adult. Spine (Phila Pa 1976) 2006;31:2109-14. [Crossref] [PubMed]
- Bess S, Protopsaltis TS, Lafage V, et al. Clinical and Radiographic Evaluation of Adult Spinal Deformity. [PubMed]
- Guerin P, Obeid I, Gille O, et al. Sagittal alignment after single cervical disc arthroplasty. J Spinal Disord Tech 2012;25:10-6. [Crossref] [PubMed]
- Jagannathan J, Shaffrey CI, Oskouian RJ, et al. Radiographic and clinical outcomes following single-level anterior cervical discectomy and allograft fusion without plate placement or cervical collar. J Neurosurg Spine 2008;8:420-8. [Crossref] [PubMed]
- Boissiere L, Takemoto M, Bourghli A, et al. Global tilt and lumbar lordosis index: two parameters correlating with health-related quality of life scores-but how do they truly impact disability? Spine J 2017;17:480-8. [Crossref] [PubMed]


