
Minimally invasive stabilization of the fractured ankylosed spine: a comparative case series study
Introduction
Fractures of the ankylosed spine are increasing in incidence and present treating physicians with numerous problems (1). Both diffuse idiopathic skeletal hyperostosis (DISH) and ankylosing spondylitis (AS) affect the axial skeleton making it more rigid which on the background of increased osteoporosis makes them more susceptible to injuries even after minor trauma (2,3). These have a higher rate of spinal cord injury and more risk of significant complication and mortality than fractures of a non-ankylosed spine (4). The long “lever arm” of these fractures, and a potential high risk of non-union and fracture displacement with conservative treatment has led to surgery being preferred in many centers. However, there is evidence that about a third are still treated conservatively (5), largely due to the increased risk of surgical complications in a generally elderly population. Coupled with the risk of surgical complications the post injury mortality in these patients is 18% at 3 months in AS (5). Furthermore, there are several reports of in-hospital deterioration in the neurological status of patients with ankylosed spines (6). Despite the risk, Robinson et al, have reported an improved survival in patients with AS that undergo surgical stabilization (7).
In thoracolumbar fractures the traditional open techniques have resulted in good results but require long segment fixation, and therefore long operative time and extensive open incisions which may increase the risk of complications. Recently there have been some case series and case reports on the use of minimally invasive surgery (MIS) utilizing percutaneous pedicle screw and rod fixation for the stabilization of these fractures (8-10). These coupled with a recent comparative case series paper have suggested that there may be an advantage in the management of these complex injuries using the MIS method.
The aim of this study is to compare the results of MIS stabilization with traditional open techniques in thoracolumbar fractures of spines with an ankylosing disorder.
Methods
A prospective ethically approved database (Spine Tango) was retrospectively reviewed to identify patients who had undergone stabilization of fractures of an ankylosed spine in the period 2010 (commencement of the database) to 2017. This list was then cross checked with the theatre database at a tertiary referral center to identify all patients who underwent surgical stabilization of their spine in the same period. Radiological studies including X-rays, CT scans and MRI scans were then reviewed to confirm the diagnosis of an ankylosed spine. Information collected included injury level, ASIA score, time in theatre, recorded blood loss in theatre, number of levels stabilized and the number of screws inserted, ASA grade and pre and post op hemoglobin. Where possible final radiographs and CT Scans were reviewed for bony union of the fracture. Medical records and Spine Tango follow-up data were reviewed for information relating to complications following surgery.
Minimally invasive surgical technique
Since 2012 the senior author (M Selby) has used MIS as a preferential technique for fixation of fractures of the ankylosed spine. Prior to this time all operative cases were performed with open techniques.
For the MIS technique at our institute we perform a pre-operative X-ray to assess the ability to visualize the pedicles on plain fluoroscopy. If the pedicles can be visualized, then MIS surgery is feasible. In all patients undergoing MIS the VIPER 2 instrumentation (DepuySynthes Raynham, MA, USA) was inserted and with osteoporotic patients having cement augmentation via the pedicle screw cannulation (Confidence-DepuySynthes Raynham, MA, USA).
We positioned patients prone and used the Wilson frame (Mizuho Osi, Union City, California, USA) if a pre-existing global kyphosis was present to avoid hyperextension of the fracture. For patients with no significant global kyphosis a standard Jackson Table is utilized (Mizuho Osi, Union City, California, USA).
Standard percutaneous pedicle screw instrumentation was undertaken, typically bilaterally 3 levels above and below the fracture using biplanar fluoroscopy. This screw insertion technique has been well described (11).
In the ankylosed spine pedicle visualization can be challenging on fluoroscopy. Therefore, after tapping the pedicle the walls of the pedicle were additionally palpated under fluoroscopic visualization.
Rod contouring needs to be accurate to avoid hyperextension at the fracture site. The rod is advanced sub-facially from cranial to caudal as the distal pedicle screws tend to be of larger diameter and soft tissue coverage is greater distally. Careful checking of rod passage both by palpation and fluoroscopy is required for the MIS technique.
If required for decompression a mini-open laminectomy is undertaken using the spinous process osteotomy (12) via a 3–4 cm separate midline incision.
For the open technique standard pedicle screw and rod instrumentation was utilized (AO USS 2 and AO URS-DepuySynthes, Raynham, MA, USA).
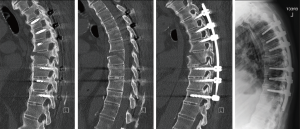
Patients are mobilized immediately post-operatively if possible and a post-operative CT scan is performed to assess screw position and fracture reduction. Patients would then be discharged when fit although all with a pre-existing neurological deficit received inpatient rehabilitation. All patients were followed up until bony union or death.
Results
We identified 17 patients who met the study inclusion criteria. We identified 10 who were stabilized using MIS techniques and 7 who were stabilized with open techniques. Demographics of the two groups are displayed in Table 1. These were similar except for age being significantly higher in the MIS group. The number of levels was similar between the two groups. Most of the patients had AS (13) rather than DISH.
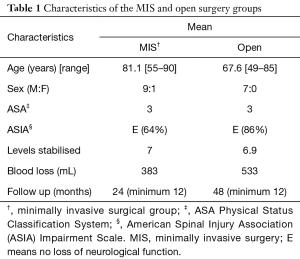
Full table
There was a significant difference in terms of pre-op vs. post-op hemoglobin level (P=0.00079) in favor of surgery performed using the MIS technique and there was a trend towards significance in favor of the MIS surgery in operating room time. There was no difference in the levels stabilized and the number of screws inserted. There was a statistically significant increase in the amount of radiation exposure to the surgeon with the MIS technique (P=0.006). There was blood transfusion seen in two patients in the open group following surgery both requiring two units. One patient in the MIS group required a pre-operative blood transfusion but none required a post-operative transfusion (Table 2).
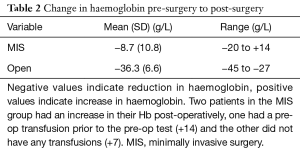
Full table
All the MIS cases had a post-operative CT scan, as is the senior authors standard practice. These scans were then reviewed for pedicle screw accuracy as per Mobbs Raley method (11). We found that 97% of screws inserted were Mobbs Raley grade 0 (within cortex of pedicle); 3% grade 1 (screw thread breach ≤2 mm of pedicle), 0% grade 2 (significant breach >2 mm without neurological compromise) and 0% grade 3 (fracture, neurological or vascular complication). No screws in the MIS group needed to be revised or removed.
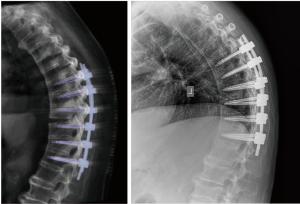
All patients in both groups demonstrated complete bony union clinically and radiologically (via CT scan) at a minimum of 12 months following surgery. This was despite some fractures being reduced in mild hyper-extension in both groups (Figure 1).
In this study group we had one patient, aged 91, who had MIS fixation die 14 days post stabilization from their medical comorbidities. One patient in the MIS group developed a superficial infection at one of the percutaneous wound sites requiring oral antibiotic and dressing treatment. One MIS patient developed a deep infection 9 months after surgery following an admission to ICU for a separate medical event and subsequent line related sepsis—this was treated medically with long term antibiotic treatment and retention of metalwork (and is now >24 months following surgery). In the open group, one patient required further surgery due to a proximal junctional fracture with displacement and neurological compromise and another patient died from pulmonary complications 9 days post-surgery.
Discussion
This comparative case series supports the use of MIS techniques in the management of thoracolumbar fractures in an ankylosed spine. Time in theatre and blood loss would suggest that this surgical technique may offer some benefits over the traditional open method.
Whilst we are advocates of the MIS techniques there are some issues which may need to be considered. We did experience some loss of reduction of the fracture position in this cohort of patients managed with MIS techniques. This was felt to occur due to the contour of the rod not being curved enough to accommodate the patients pre-existing deformity. We can report that this patient despite the slight extension of the fracture did go on to unite their fracture (Figure 2).
The radiation exposure in our series was significantly increased in the MIS group. Methods to reduce the radiation the surgeon experience would be beneficial due to the reported incidence of thyroid cancer and cataracts. We would advocate wearing full lead including thyroid shield and lead eye protection where possible. Methods such as navigation may also help reduce this but are not currently available in our institution.
It has been shown in several studies and in two systematic reviews that MIS surgery is superior to open techniques in general (12-16). It has been shown to reduce the length of stay, reduce the intra-operative blood loss and reduce operative time. Our results would support this in the setting of the ankylosed spine. We feel our blood loss would have been even lower if there had not been the clinical need to perform a laminectomy on two of the MIS patients which increased the reported blood loss. This is supported by the recent publication which has shown that there was a clinically significant difference in transfusion rates between the MIS group and open group (17).
Limitations of this study are the small size of the patient groups. Despite this, we feel that the results can still be supportive of the use of this method of stabilization in this population. Another limitation is that not all blood loss can be quantified in MIS cases. We therefore compared pre-op and post-op hemoglobin levels and looked at the need for blood transfusion after surgery. Whilst a drop in hemoglobin was statistically significant between the groups, blood transfusion rates were not.
Overall, we feel this paper adds to the growing evidence of the use of MIS techniques in the challenging setting of thoracolumbar fractures in the ankylosed spine. There may be a further benefit to the healthcare provider in shortened length of stay. Unfortunately, this study was not able to assess this due to the low number of patients and several confounds amongst the patient population.
Conclusions
The surgically demanding MIS technique may offer benefits to the patient and appears to be comparable to the open technique. Further evidence to support this method is required in terms of larger studies.
Acknowledgements
The authors thank Leeanne Gladigau for her maintenance of the Spine Tango Database at the Royal Adelaide Hospital.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethics approval was not required for this study. Consent was obtained from all patients.
References
- Robinson Y, Sanden B, Olerud C. Increased occurrence of spinal fractures related to ankylosing spondylitis: a prospective 22-year cohort study in 17,764 patients from a national registry in Sweden. Patient Saf Surg 2013;7:2. [Crossref] [PubMed]
- Heyde CE, Fakler JK, Hasenboehler E, et al. Pitfalls and complications in the treatment of cervical spine fractures in patients with ankylosing spondylitis. Patient Saf Surg 2008;2:15. [Crossref] [PubMed]
- Choi D. Fractures in Ankylosing Disorders of the Spine: Easy to Miss and High Risk of Deterioration. World Neurosurg 2015;83:1029-31. [Crossref] [PubMed]
- Westerveld LA, van Bemmel JC, Dhert WJ, et al. Clinical outcome after traumatic spinal fractures in patients with ankylosing spinal disorders compared with control patients. Spine J 2014;14:729-40. [Crossref] [PubMed]
- Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: a systematic review of the literature on treatment, neurological status and complications. Eur Spine J 2009;18:145-56. [Crossref] [PubMed]
- Schiefer TK, Milligan BD, Bracken CD, et al. In- Hospital neurologic deterioration following fractures of the ankylosed spine: a single-institution experience. World Neurosurg 2015;83:775-83. [Crossref] [PubMed]
- Robinson Y, Willander J, Olerud C. Surgical Stabilization improves survival of Spinal fractures related to Ankylosing Spondylitis. Spine 2015;40:1697-702. [Crossref] [PubMed]
- Yeoh D, Moffatt T, Karmani S. Good Outcomes of percutaneous fixation of Spinal fractures in Ankylosing spinal disorders. Injury 2014;45:1534-8. [Crossref] [PubMed]
- Nayak Nr, Pisapia JM, Abdullah KG, et al. Minimally invasive surgery for traumatic fractures in Ankylosing spinal disease. Global Spine J 2015;5:266-73. [Crossref] [PubMed]
- Krüger A, Frink M, Oberkircher L, et al. Percutaneous dorsal instrumentation for thoracolumbar extension-distraction fractures in patients with ankylosing spinal disorders: a case series Spine J 2014;14:2897-904. [Crossref] [PubMed]
- Raley D, Mobbs R. Retrospective Computed Tomography Scan Analysis of Percutaneously Inserted Pedicle Screws for Posterior Transpedicular Stabilization of the Thoracic and Lumbar Spine: Accuracy and Complication Rates. Spine 2012;37:1092-100. [Crossref] [PubMed]
- Weiner BK, Fraser RD, Peterson M. Spinous Process Osteotomies to Facilitate lumbar decompressive surgery. Spine 1999;24:62-6. [Crossref] [PubMed]
- Fitschen-Oestern S. Reduction and retention of thoracolumbar fractures by minimally invasive stabilization versus open posterior instrumentation. Injury 2015;46:S63-70. [Crossref] [PubMed]
- Elsawaf AM. Outcome of Percutaneous versus open posterior spinal fixation in thoracolumbar fractures. Neurosurgery 2016;63:196. [Crossref]
- McAnany SJ, Overley SC, Kim JS, et al. Open versus minimally invasivefixation techniques for thoracolumbar trauma: A meta-Analysis. Global Spine J 2016;6:186-94. [Crossref] [PubMed]
- Phan K, Rao PJ, Mobbs RJ. Percutaneous versus open pedicle screw fixation for treatment of thoracolumbar fractures: Systematic review and meta-anlayiss of comparative studies. Clin Neurol Neurosurg 2015;135:85-92. [Crossref] [PubMed]
- Sedney CL, Daffner SD, Obafemi-Afolabi A, et al. A comparision of Open and Percutaneous techniques in the operative fixation of spinal fractures associated with Ankylosing spinal disorders. Int J Spine Surg 2016;10:23. [Crossref] [PubMed]


