
Predicting critical care unit-level complications after long-segment fusion procedures for adult spinal deformity
Introduction
Adult spinal deformity (ASD) has been increasingly recognized as an important cause of pain and disability, particularly in the elderly population (1). The etiology of ASD can be variable and include degenerative, idiopathic, and iatrogenic causes but also can present as a progression of adolescent scoliosis. Surgery, although not without major risks, has been shown to provide excellent outcomes in most patients (2-5). While corrective surgeries are considered relatively safe procedures, major complications such as reintubation, myocardial infarction, cardiac arrest, among others, may still occur.
The modified Clavien-Dindo classification system was developed in 2004 as a tool to help clinicians identify and describe surgical complications (6). This system categorizes postoperative complications into five grades, depending on the severity and, more importantly, on the therapy required to treat such complications (6). For example, Grade II complications include pneumonia or arrhythmia, both of which can be treated with medications. On the other hand, Grade 4 complications, including respiratory failure requiring intubation, or new stroke, require critical/intensive care and are usually defined as life-threatening.
The American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) is a prospective surgical database developed as a tool to help identify patients at highest risk of postoperative complications, in an effort to reduce healthcare costs and improve treatment quality. Multiple studies have used it to identify patients at higher risk for complications after spine surgery (7-11), but there is limited data on complications requiring critical care. Thus, the purpose of the present study was to develop a predictive model to identify patients at risk for Clavien-Dindo Grade 4 complications, specifically after long-segment fusion procedures for ASD.
Methods
Study design and data source
This is a case-control retrospective study utilizing the ACS-NSQIP databases from 2010 to 2014 (https://www.facs.org/quality-programs/acs-nsqip). This study was deemed exempt from review by the local institutional review board [2016-6862]. NSQIP is a surgical database from over 500 hospitals in the United States that collects perioperative and 30-day follow-up data on randomly assigned cases. A trained surgical reviewer at each participating hospital collects data via chart reviews, letters, and/or phone calls. The current success rate in data capture and inter-rater reliability for all variables is approximately 95% (12).
Collected data
Adult patients over 18 years of age with a principal diagnosis of spinal deformity were first identified via use of ICD-9 codes for kyphosis (737.10), acquired postural kyphosis (737.10), postlaminectomy kyphosis (737.12), other acquired kyphosis (737.19), kyphoscoliosis (737.3), idiopathic kyphoscoliosis (737.30), thoracogenic scoliosis (737.34), and other kyphoscoliosis (737.39). Only patients who underwent fusion of 7 or more spinal segments were identified via the CPT codes 22802, 22743, 22804, and/or 22844. Patients with ventilator dependency (n=5), cancer (n=3), quadraparesis (n=3), and history of previous stroke with neurological deficit (n=3) were excluded from this study.
Collected patient data included age, sex, body mass index (BMI), smoking status, history of chronic obstructive pulmonary disease, hypertension, diabetes, congestive heart failure, chronic steroid use, bleeding disorder, dependent functional status (requiring assistance from others for activities such as bathing, dressing, mobility, feeding, and toileting), preoperative albumin, and preoperative hematocrit.
Examined operative parameters included revision status, laminectomy, interbody fusion, use of osteotomy, use of three-column osteotomy (3CO), pelvic fixation, combined anterior/posterior approaches, operative time, and use of blood transfusion.
Outcome measures
The primary outcome measure was development of at least one critical care unit (CCU)-level complication. Based on the Clavien-Dindo definition, these complications included intraoperative arrest/infarction, ventilation >48 hours, pulmonary embolism, renal failure requiring dialysis, cardiac arrest, myocardial infarction, unplanned intubation, septic shock, stroke, coma, or the occurrence of new neurological deficits (6,13,14).
Statistical analysis
All analyses were performed on Stata SE 12 (Stata Corp., College Station, Texas, USA). Descriptive statistics were used to describe the study population and comparison between groups (CCU vs. No-CCU) was done via t-tests or Pearson chi-squared tests. A stepwise multivariate logistic regression analysis with backward elimination was performed to identify significant predictors of CCU complications. Results are presented as odds ratios (OR) with 95% confidence intervals (CI). Significant predictors were used to construct the final predictive model and the area under the receiver operating characteristic curve (AUROC) was calculated. Statistical significance was set at P<0.05.
Results
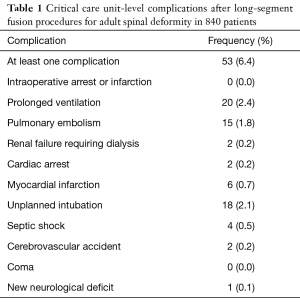
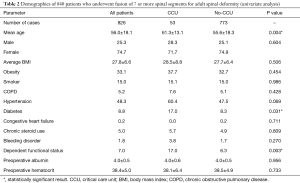
A total of 826 patients who underwent more than 7-level fusion for ASD were included in this study, 53 of whom (6.4%) developed at least one CCU complication. The most common complication was prolonged ventilation (2.4%), followed by unplanned intubation (2.1%) and pulmonary embolism (1.8%) (Table 1). The average age of all patients was 56.0±18.1 years and 74.7% were female. Between the CCU and No-CCU groups, there were significant differences in age (61.3±13.1 vs. 55.6±18.3, P=0.004), prevalence of diabetes (17.0% vs. 8.3%, P=0.031), and prevalence of dependent functional status (17.0% vs. 6.3%, P=0.003) (Table 2).
Full table
Full table
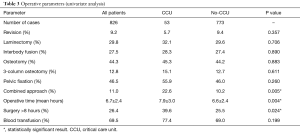
Operative parameters were relatively similar between groups (Table 3). However, there were significant differences in the proportion of patients who underwent a combined approach (22.6% in the CCU group vs. 10.2% in the No-CCU group, P=0.005) and who underwent surgery for over 8 hours (39.6% vs. 25.5%, P=0.024).
Full table
Model construction
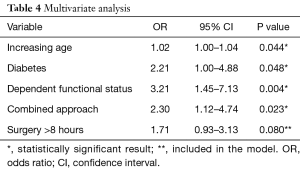
All factors with a P value less than 0.05 on univariate analysis were included in a stepwise multivariate logistic regression analysis with backward elimination to construct the predictive model (Table 4). Factors that were used to construct the model included dependent functional status (P=0.004), combined approach (P=0.023), age (P=0.044), diabetes (P=0.048), and surgery for over 8 hours (P=0.080). Although long operative time did not reach statistical significance, this parameter was included in the final model due to the growing body of evidence suggesting its association with worse short-term outcome after spine surgery (7,15,16).
Full table
The final model assigned 2 points for dependent functional status, 1 point for combined approach, 1 point for diabetes, and 1 point for surgery >8 hours. Furthermore, we subdivided age in subgroups assigning 0 points for patients aged <50, 1 point for patients between 50–70, 2 points for patients 70 or over (Table 5). The minimum score is 0 and the maximum is 7. The numeric point assignment was based on the relative P value on multivariate analysis.
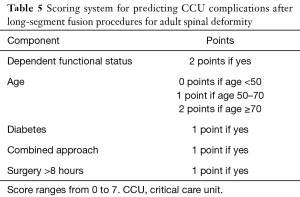
Full table
Association of predictive model with outcome
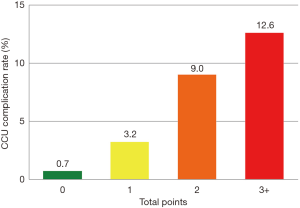
There were 142 patients with 0 points (17.2%), 253 with 1 point (30.6%), 288 with 2 points (34.9%), and 143 patients with 3 or more points (17.3%); there was a significant increase in CCU complications with increasing points (P<0.001) (Figure 1): the rates of CCU complications was 0.7%, 3.2%, 9.0%, and 12.6% for patients with 0, 1, 2, and 3+ points, respectively (P<0.001). The AUROC was calculated at 0.721.
Discussion
Although surgical ASD correction has been shown to provide substantial benefits in terms of pain, self-image, quality of life, and function compared to non-operative treatment (17-19), surgery has been associated with significant morbidity and economic costs (2,20). As a consequence, efforts have been made to reduce postoperative complications, including identification of patient and/or operative risk factors to use in the surgical decision-making process (10,21,22). However, there is limited data about risk factors for CCU complications. The main objective of this investigation is to address this shortcoming.
We examined 826 patients who underwent adult scoliosis and found a 6.4% CCU complication rate. Logistic regression analysis then revealed five factors to be the strongest predictors of CCU events, including patient age, diabetes, dependent functional status, combined approach and length of surgery. The final predictive model assigned various points for each parameter, ranging from 0 to a maximum of 7 points. Complication rates significantly increased with increasing points. Although multiple studies have identified factors associated with complication occurrence after ASD surgery, our present study offers a relatively simple 5-element scoring system that could potentially be the foundation for future predictive models, particularly for CCU complications.
Patient age has been shown in multiple studies to be associated with worse outcomes after spine surgery (8,9,23-25). Phan et al. examined 5,095 patients who underwent surgery for adult scoliosis, finding 30-day complication rates of 19.4%, 21.8%, 27.4%, and 31.4% for patients aged <52, 53–61, 62–69, and 70 or older, respectively (P<0.001) (9). In their study, they postulated that while chronological age and biological age are not directly correlated, the former may still be used as a valuable tool for preoperative risk stratification (9).
The second parameter that was included in our predictive model was diabetes. This comorbidity is currently one of the top 10 causes of mortality in the United States, with an estimated prevalence of approximately 9% of the population (26). Several studies have also suggested an increase in perioperative complications after spinal surgery (27-29). Klemencsics et al. examined 1,030 patients who underwent elective routine lumbar spine surgery, and found a surgical site infection rate of 3.5%. Multivariate analysis to build a predictive model identified diabetes as an independent predictor for infections (27). Similarly, Bohl et al. found both non-insulin and insulin-dependent diabetes to be significant risk factors for postoperative pneumonia after lumbar spine surgery, with relative risks of 2.4 and 2.9, respectively (29).
Preoperative functional status, as assessed in the NSQIP database, indicates whether a person requires assistance for activities of daily living. While it may be the result of a patient’s baseline comorbidities or severe spinal deformity leading to pain/disability, a recent study examining 1,247 patients who underwent deformity surgery found that being dependent on others increased the risk of major postoperative complications by a factor of 2.09 after multivariate adjustment (17.1% rate in dependent patients and 9.2% in independent patients, P=0.0200) (7).
Lastly, combined approaches and long operative time were also associated with CCU complications in our study. Pourfeizi et al. compared 25 patients treated via a posterior approach to 25 patients treated via a combined approach for the treatment of scoliotic curves of over 70 degrees (30). The authors found that patients treated via combined approaches had significantly longer total lengths of stay (26.5 vs. 11.8 days, P<0.001) and intensive care unit stay (4.7 vs. 1.5 days, P<0.001) (30). Prolonged operative time (defined as over 8 hours in our study) has also shown to be an important predictor of perioperative complications (7,31,32); Puffer et al., for example, showed that both total operative time and anesthetic time were associated with wound infection following spine surgery (31). Prolonged operative time leaves the wound exposed for longer periods of time, is associated with higher blood loss, prolonged anesthetic use, and others, all of which could contribute to the increased rate of complications after deformity surgery.
Overall, the findings of the present study may provide the foundation towards a clinical predictive model to assist patients and clinicians in preoperative risk stratification for deformity surgery, particularly for complications that may require critical care or are potentially life threatening. Although NSQIP has built a risk calculator for all surgical procedures (http://riskcalculator.facs.org/RiskCalculator/), our current model is tailored to long-segment fusion procedures for scoliosis, with an AUROC of 0.702 suggesting good model fit. Nonetheless, there are limitations to the use of this database for spine surgery patients, such as lack of radiographic parameters or more specific clinical findings. Although there was a significant stepwise association between increasing score and complications, other unmeasured variables may alter the results, and future validation is needed.
Conclusions
A scoring system for patients undergoing long-segment fusion procedures for ASD was built and shown to predict 30-day complications requiring critical care. Although future research is needed to corroborate our findings, this may provide a framework for identification of patients at highest risk for major complications following deformity surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The abstract of this manuscript was presented as an electronic poster in Congress of Neurological Surgeon’s Annual Meeting 2017 in Boston Massachusetts, October 7–11, 2017.
Ethical Statement: This study was deemed exempt from review by the local institutional review board [2016-6862]. The ACS-NSQIP and the hospitals participating in the ACS-NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
References
- Ames CP, Scheer JK, Lafage V, et al. Adult Spinal Deformity: Epidemiology, Health Impact, Evaluation, and Management. Spine Deform 2016;4:310-22. [Crossref] [PubMed]
- Sciubba DM, Yurter A, Smith JS, et al. A Comprehensive Review of Complication Rates After Surgery for Adult Deformity: A Reference for Informed Consent. Spine Deform 2015;3:575-94. [Crossref] [PubMed]
- Smith JS, Klineberg E, Lafage V, et al. Prospective multicenter assessment of perioperative and minimum 2-year postoperative complication rates associated with adult spinal deformity surgery. J Neurosurg Spine 2016;25:1-14. [Crossref] [PubMed]
- Smith JS, Lafage V, Shaffrey CI, et al. Outcomes of Operative and Nonoperative Treatment for Adult Spinal Deformity: A Prospective, Multicenter, Propensity-Matched Cohort Assessment With Minimum 2-Year Follow-up. Neurosurgery 2016;78:851-61. [Crossref] [PubMed]
- Smith JS, Shaffrey CI, Berven S, et al. Improvement of back pain with operative and nonoperative treatment in adults with scoliosis. Neurosurgery 2009;65:86-93; discussion 93-4. [Crossref] [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- De la Garza Ramos R, Goodwin CR, Elder BD, et al. Preoperative functional status as a predictor of short-term outcome in adult spinal deformity surgery. J Clin Neurosci 2017;39:118-23. [Crossref] [PubMed]
- De la Garza Ramos R, Goodwin CR, Passias PG, et al. Timing of Complications Occurring Within 30 Days After Adult Spinal Deformity Surgery. Spine Deform 2017;5:145-50. [Crossref] [PubMed]
- Phan K, Kim JS, Somani S, et al. Impact of Age on 30-day Complications After Adult Deformity Surgery. Spine (Phila Pa 1976) 2018;43:120-6. [Crossref] [PubMed]
- Di Capua J, Somani S, Kim JS, et al. Hospital-Acquired Conditions in Adult Spinal Deformity Surgery: Predictors for Hospital-Acquired Conditions and Other 30-Day Postoperative Outcomes. Spine (Phila Pa 1976) 2017;42:595-602. [Crossref] [PubMed]
- Manoharan SR, Baker DK, Pasara SM, et al. Thirty-day readmissions following adult spinal deformity surgery: an analysis of the National Surgical Quality Improvement Program (NSQIP) database. Spine J 2016;16:862-6. [Crossref] [PubMed]
- Shiloach M, Frencher SK Jr, Steeger JE, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 2010;210:6-16. [Crossref] [PubMed]
- Schwab FJ, Hawkinson N, Lafage V, et al. Risk factors for major peri-operative complications in adult spinal deformity surgery: a multi-center review of 953 consecutive patients. Eur Spine J 2012;21:2603-10. [Crossref] [PubMed]
- Abt NB, Richmon JD, Koch WM, et al. Assessment of the Predictive Value of the Modified Frailty Index for Clavien-Dindo Grade IV Critical Care Complications in Major Head and Neck Cancer Operations. JAMA Otolaryngol Head Neck Surg 2016;142:658-64. [Crossref] [PubMed]
- Bernstein DN, Thirukumaran C, Saleh A, et al. Complications and Readmission After Cervical Spine Surgery in Elderly Patients: An Analysis of 1786 Patients. World Neurosurg 2017;103:859-68.e8. [Crossref] [PubMed]
- Saleh A, Thirukumaran C, Mesfin A, et al. Complications and readmission after lumbar spine surgery in elderly patients: an analysis of 2,320 patients. Spine J 2017;17:1106-12. [Crossref] [PubMed]
- Li G, Passias P, Kozanek M, et al. Adult scoliosis in patients over sixty-five years of age: outcomes of operative versus nonoperative treatment at a minimum two-year follow-up. Spine (Phila Pa 1976) 2009;34:2165-70. [Crossref] [PubMed]
- Smith JS, Shaffrey CI, Berven S, et al. Operative versus nonoperative treatment of leg pain in adults with scoliosis: a retrospective review of a prospective multicenter database with two-year follow-up. Spine (Phila Pa 1976) 2009;34:1693-8. [Crossref] [PubMed]
- Bridwell KH, Glassman S, Horton W, et al. Does treatment (nonoperative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis: a prospective multicenter evidence-based medicine study. Spine (Phila Pa 1976) 2009;34:2171-8. [Crossref] [PubMed]
- Zygourakis CC, Liu CY, Keefe M, et al. Analysis of National Rates, Cost, and Sources of Cost Variation in Adult Spinal Deformity. Neurosurgery 2018;82:378-87. [Crossref] [PubMed]
- Scheer JK, Smith JS, Schwab F, et al. Development of a preoperative predictive model for major complications following adult spinal deformity surgery. J Neurosurg Spine 2017;26:736-43. [Crossref] [PubMed]
- Passias PG, Soroceanu A, Yang S, et al. Predictors of Revision Surgical Procedure Excluding Wound Complications in Adult Spinal Deformity and Impact on Patient-Reported Outcomes and Satisfaction: A Two-Year Follow-up. J Bone Joint Surg Am 2016;98:536-43. [Crossref] [PubMed]
- Carreon LY, Glassman SD, Shaffrey CI, et al. Predictors of Health-Related Quality-of-Life After Complex Adult Spinal Deformity Surgery: A Scoli-RISK-1 Secondary Analysis. Spine Deform 2017;5:139-44. [Crossref] [PubMed]
- Elsamadicy AA, Adogwa O, Reddy GB, et al. Risk Factors and Independent Predictors of 30-Day Readmission for Altered Mental Status After Elective Spine Surgery for Spine Deformity: A Single-Institutional Study of 1090 Patients. World Neurosurg 2017;101:270-4. [Crossref] [PubMed]
- Gum JL, Lenke LG, Bumpass D, et al. Does Planned Staging for Posterior-Only Vertebral Column Resections in Spinal Deformity Surgery Increase Perioperative Complications? Spine Deform 2016;4:131-7. [Crossref] [PubMed]
- Statistics About Diabetes. 2017. Available online: http://www.diabetes.org/diabetes-basics/statistics/?referrer=https://www.google.com/
- Klemencsics I, Lazary A, Szoverfi Z, et al. Risk factors for surgical site infection in elective routine degenerative lumbar surgeries. Spine J 2016;16:1377-83. [Crossref] [PubMed]
- Salmenkivi J, Sund R, Paavola M, et al. Mortality Caused by Surgery for Degenerative Lumbar Spine. Spine (Phila Pa 1976) 2017;42:1080-7. [Crossref] [PubMed]
- Bohl DD, Mayo BC, Massel DH, et al. Incidence and Risk Factors for Pneumonia After Posterior Lumbar Fusion Procedures: An ACS-NSQIP Study. Spine (Phila Pa 1976) 2016;41:1058-63. [Crossref] [PubMed]
- Pourfeizi HH, Sales JG, Tabrizi A, et al. Comparison of the Combined Anterior-Posterior Approach versus Posterior-Only Approach in Scoliosis Treatment. Asian Spine J 2014;8:8-12. [Crossref] [PubMed]
- Puffer RC, Murphy M, Maloney P, et al. Increased Total Anesthetic Time Leads to Higher Rates of Surgical Site Infections in Spinal Fusions. Spine (Phila Pa 1976) 2017;42:E687-90. [Crossref] [PubMed]
- Kothari P, Somani S, Lee NJ, et al. Thirty-Day Morbidity Associated with Pelvic Fixation in Adult Patients Undergoing Fusion for Spinal Deformity: A Propensity-Matched Analysis. Global Spine J 2017;7:39-46. [Crossref] [PubMed]


