
Bowel injury in lumbar spine surgery: a review of the literature
Introduction
Bowel injury is considered a rare but serious complication of spine surgery associated with high morbidity and mortality rates due to severe intra-abdominal sepsis and shock. Bowel injury can be defined as trauma associated with the intestinal wall ranging from incomplete injury, such as a simple abrasion, to complete injury which includes perforation of the bowel. It is estimated that the mortality for perforation injury-related intra-abdominal sepsis ranges between 7.5% and 36% (1-4). Recent advances in spinal instrumentation have led to the development of several new minimally invasive surgical (MIS) approaches such as anterior lumbar interbody fusion (ALIF), direct or indirect lateral interbody fusion (LIF), and transforaminal lumbar interbody fusion (TLIF). These procedures contribute to minimizing the size and number of incisions and the extent of tissue retraction, as well as reducing surgical time, blood loss, and length of hospital stay (5-10). However, even with these new techniques and safeguards, cases of bowel perforation injury are reported in the current literature.
Our goal was to evaluate cases of bowel perforation injury concurrent with lumbar spine surgery as well as the causes and any possible means of avoidance.
Patient and methods
We performed a literature search in the PubMed database using the following terms: “abrasion,” “bowels,” “bowel,” “complication,” “injury,” “intestine,” “intra-abdominal sepsis/shock,” “perforation,” “lumbar,” “spine,” “surgery,” and “visceral.” These terms were used alone and in every possible combination. The search was limited to English language articles and abstracts published between January 1960 and March 2016. In each case, the diagnostic criteria, outcomes, risk factors, surgical approach, and the treatment strategy that was followed were recorded.
Results
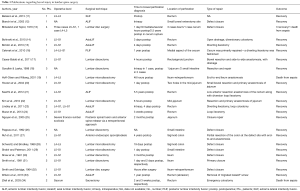
Twenty-four publications were included in our analysis with a total of 31 reported cases of bowel injury (11-34) (Table 1). In one article, the authors described a case of abrasion of the rectum and symptoms of tenesmus without complete injury after an axial lumbar interbody fusion (AxiaLIF) procedure (33). Twelve publications described bowel injury following lumbar disc surgery or lumbar microdiscectomy (13,17-20,22,26,28-32). In one publication, bowel injury occurred during sacrectomy for tumor removal (34). There were 10 publications in which bowel injury was described after lateral approaches and MIS spinal procedures in the lumbar spine (11,12,14-16,21,23,24,27,33). Additionally, one study reported bowel injury after instrumentation failure in a procedure for a spinal deformity (25).
Full table
The surgical procedures involved in the bowel injuries were discectomy (13,17,18,26,30-32), microdiscectomy (19,20,22,28,29) extreme lateral interbody fusion (XLIF) (11), AxiaLIF (14,15,23,24,33), ALIF (12,21), anterior endoscopic spondylodesis at L5–S1 (27) posterior lumbar interbody fusion (PLIF) (16), posterior spinal fusion-anterior spine release through a retroperitoneal approach (25), and sacrectomy (34). An analysis of the types of surgeries that these patients underwent demonstrated that bowel injury was more frequent in lumbar discectomy and microdiscectomy (18 of 31 patients, 58.1%). MIS and lateral techniques such as ALIF, XLIF, and TLIF were the second most common with 10 cases (32.3%). Sacrectomies (6.5%) and posterior fusion plus ALL release (3.2%) had the lowest number of reported bowel complications.
In all cases, timing of the injury was an important factor and played an important role in determining the diagnosis after injury. In most cases, bowel injury occurred during surgery and was noted at the time. Three cases of bowel injury were diagnosed postoperatively due to migration of instrumentation (16,21,27). Abrasion of the intestinal wall in one patient was the result of a migrated screw after a lumbosacral AxiaLIF procedure (33).
Because all reported cases involved the lumbosacral spine, we studied the operative levels and locations that were most commonly associated with bowel injury and found that bowel injury was most common at L5–S1 (15 of 31 patients, 48.4%), followed by the L4–L5 level (5 of 31 patients, 16.1%). Two cases were noted in conjunction with sacral surgery (6.5%) (34). In 6 cases (19.4%), the level was not identifiable in the reports (12,18,25,26). Seventeen cases of injury (54.8%) occurred in the small intestine, 9 (29.0%) in the rectum, and 5 (16.1%) in the cecum, sigmoid, or rectosigmoid area.
Time to diagnosis was categorized as intraoperative (3 of 31 patients, 9.7%) (12,18,23), less than 48 hours after surgery (12 of 31 patients, 38.7%) (11,13,17,18,20,22,29,31,32), 48 hours to 1 week after surgery (5 of 31 patients, 16.1%) (14,15,19,23,31), 1 week to 1 year after surgery (6 of 31 patients, 19.3%) (24,25,28,30,34), and more than 1 year after surgery (4 of 31 patients, 12.9%) (13,21,27,33). One article did not specify the time of bowel injury (26). Acute abdominal pain, hyperemesis, hypotension, and peritonitis with subsequent sepsis were the clinical findings in most patients (17,18,25,28,31). Other clinical findings included haemorrhage (15,34), tenesmus (33), edema, or inflammation at the site of the injury due to communication with the intestine; abscess (14,16,32); and discovering parts of instrumentation in the feces (21,27). Radiological evaluation plus computed tomography (CT) of the abdomen in these cases revealed intra-abdominal fluid and pneumoperitoneum, intestinal fistulas, or abdominal abscesses, and instrumentation close to the gastrointestinal tract. Also, rectal imaging techniques were used in some cases in which rectal injury was suspected (33). Patients underwent either restoration of the bowel injury immediately intraoperatively (12,13,18,23) or secondarily if the lesion was detected soon after the spine procedure (15-17,19-22,24,29). The type of procedures patients underwent for bowel repair were defect closure, end-to-end anastomosis plus external drainage, resection plus anastomosis, and ileostomy/colostomy (12-15,17-26,28-32,34). There were also cases with chronic inflammatory findings (abscess or fistula) that were treated after the main surgery (16,27). The overall morbidity rate from bowel injury was 87.1% (27 of 31 patients). The mortality rate was 12.9% (4 of 31 patients) due to irreversible sepsis (13,19,34).
Discussion
Surgical approaches for the treatment of disease of the lumbosacral spine can be divided into percutaneous, endoscopic, and arthrodesis procedures (35,36). Percutaneous techniques were developed in the 1960s and 1970s (37,38). Endoscopic lumbar techniques were introduced in the 1980s and 1990s (39-41). Lumbar arthrodesis procedures, such as posterior fixation with pedicle screws, TLIF, ALIF, direct or indirect LIF, and AxiaLIF, have become increasingly more minimally invasive (42-45). Looking only at microdiscectomies over the years, between 1960 and 2000, there were five publications discussing bowel injury as a complication from surgery. In 2000–2010, there were eight publications reporting bowel injury; and from 2010 until March 2016, eight publications documented bowel injury in the medical literature as well. Looking at the evolution of MIS procedures for the lumbar spine, we found that bowel injury remains a rare complication, described mostly anecdotally in case reports.
Aside from direct injury to the intestines during surgical manipulations, migration and instability of a fusion construct was documented as having played an important role in a bowel injury event (16,21,25,27). With new advances and variability in MIS approaches, techniques, devices, and constructs, the risk of bowel injury appears to be increasing. Failure of interbody fusions or anterior displacement of cages can lead to bowel injury and spinal instability. Bowel injury rates would logically make sense as a marker of the learning curve for surgeons with each new lumbar spine procedure that is introduced, although this is not necessarily supported by the literature (18,31).
In recent years, registries including the Society of Lateral Access Surgery (SOLAS) and the International Spine Study Group have been working diligently toward recording the outcomes of surgical procedures and their associated complications, such as bowel injury. Uribe et al. compiled the results of a survey of the complications occurring during lateral lumbar spine approaches performed by experienced (more than 100 cases) MIS-LIF surgeons participating in the SOLAS registry (46). These authors concluded that the rate of bowel injuries in more than 13,000 LIF cases was 0.08% (46). However, the existing registries do not represent all MIS procedures performed and their complications.
Additional important factors in the discussion of this issue are the medicolegal implications that can arise due to bowel injury. In their unique and noteworthy study, Goodkin and Laska analyzed the legal aspects of major complications associated with lumbar disc surgery (18). They concluded that, in such circumstances, surgeons are frequently required to defend themselves in court and the occurrence of malpractice lawsuits has become a growing concern when performing such approaches (18).
Furthermore, it is a reasonable finding that the lower lumbar spine levels are the most commonly involved levels in bowel injury during spine surgery. Degenerative changes and disc herniations are commonly seen at these levels because they tend to be symptomatic and are below the conus medullaris. Because of the high volume of cases at these levels, it is understandable that the number of reported complications is slightly higher than those reported at other spinal levels.
The diagnosis of bowel injury is established by the combination of clinical and imaging findings. Interestingly, bowel injury was reported in two cases when the disc specimen retrieved during the procedure was sent to pathology and gastrointestinal mucosa was found, indicating bowel injury (13,18). Clinical findings such as peritonitis, wound infection, abdominal pelvic abscesses, enterocutaneous fistulae, and more rarely, postoperative discitis may indicate the presence of a bowel injury (18,31). Imaging studies such as abdominal X-rays and CT can show free air and fluid in the peritoneal cavity or pieces of migrated instrumentation (47). Magnetic resonance imaging (MRI) can reveal enterocutaneous fistulae and abdominal pelvic abscesses.
Risk factors for bowel injury can be divided into two categories: factors related to the surgical approach and general predisposing factors. Factors related to the surgical approach reference the means by which the surgeon is accessing the disk space, patient positioning relative to how the disk space is being accessed, use of instrumentation, surgical anatomy, use of a microscope, and the surgeon’s experience (13,18,31,48,49). General predisposing risk factors are: recurrent spine surgery, history of abdominal or rectal surgeries, preoperative irradiation, history of abdominal infections, pelvic inflammatory disease, appendicitis, or diverticulitis, which can increase the presence of abdominal adhesions (14,15,31,50).
According to published data (Table 1), in posterior approaches such as lumbar microdiscectomy and PLIF, bowel perforation could be caused after penetration of the anterior longitudinal ligament (ALL). An existing defect in the anterior part of the annulus fibrosus and the ALL or the intraoperative rupture of the internal disc wall and the ALL during surgical manipulations could lead to bowel injury (48,51). Anatomically safe working zones were developed by spine surgeons in order to avoid the possibility of injury to the lumbar plexus and vessels (52). Unfortunately, the anatomical relationship of the bowel to the lumbar spine is not as accurately defined in the literature as it is with vessels and nerves because of the mobility of the intraperitoneal organs. For example, with the patients in a prone position, the small intestine can be located in front of the L5–S1 disc space (53). The peritoneum can be traumatized by instrumentation or surgical manipulations during the lateral transpsoas approach due to its close proximity to the psoas muscle, which can lead to bowel perforation (11). Kanemura et al. investigated the possibility for a colonic perforation during an XLIF procedure by calculating the distance of the descending and ascending colon from the lateral approach pathway (54). They concluded that in 30% of their patients there was a margin between the colon and the posterior pararenal space that could increase the risk of colon perforation. According to their study, perioperative abdominal CT could provide useful information for the avoidance of this complication (54). Surgeons must divide the peritoneum from muscle layers to reach the lumbar spine in anterior retroperitoneal approaches, creating an increased risk of bowel perforation by surgical manipulations due to micro-ruptures of the peritoneum (12). The presacral AxiaLIF technique carries the greatest risk for bowel perforation injury due to the anatomical relationship of the sacral bone to the rectum (14,15). A thinner presacral space in women predisposes them to an increased risk of rectal perforation (24). Other important risk factors are rectal prolapse and thin prerectal fat (50).
Another important observation is that some spine surgeons do not remove the instrumentation after the occurrence of a bowel injury. It has been described in the literature that these patients may have an increased risk of infection (18,28,30,32). However, in several published case reports, outcomes in regards to the fusion surgery for these patients are favourable, and they do not have documented infections even with bowel injuries (11,12,14-16,21,23,24,27).
An important discussion relevant to the complication of bowel perforation is regarding methods of avoidance. The literature suggests that the primary means of avoidance is presurgical evaluation of imaging studies such as lumbar CT and MRI. These imaging studies provide useful information regarding sagittal vertebra length plus anatomical anomalies or variations that surgeons should recognize before surgery (6,13,14,53). In addition, unnecessary surgical manipulations should be avoided and the procedure should be confined to the disc space. Especially during a posterior lumbar microdiscectomy, the length of the operative disc space can be estimated using set measures to better appreciate an appropriate working depth (13). The status of the ALL can be checked with the application of normal saline in the disc space. If the same amount of saline returns and remains, rupture is less likely. Another important consideration is presurgical bowel preparation because it improves relaxation of the intestinal walls and decreases the possibility of a bowel injury (24). Also, obtaining a medical history and performing a thorough clinical examination can lead physicians to safer surgical approaches (14). The choice of instrumentation is important to provide a stable biomechanical construct in the lumbar spine (21). Furthermore, postoperative imaging can provide significant information about instrumentation complications related to pseudarthrosis and migration of instrumentation (21). Finally, in cases of large intestine and rectum perforation, there is a possibility for defect entrenchment and subsequent appearance of fistulas and abscesses (13,19,34). Treating bowel injury complications in a timely manner leads to more favourable outcomes and decreases mortality.
In conclusion, although bowel perforation in lumbar spine surgery has high percentages of morbidity and mortality, it is a rare event. Preoperative surgical planning based on clinical evaluation and medical history as well as the use of an optimal surgical approach could minimize the risks of such an event occurring. An awareness of potential complications and a higher level of suspicion allow surgeons to recognize and treat problems quickly. Early responses have been shown to improve clinical outcomes.
Acknowledgements
The authors thank Carrie Owens MSILS and Debra J. Zimmer for editorial assistance.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Mulari K, Leppaniemi A. Severe secondary peritonitis following gastrointestinal tract perforation. Scand J Surg 2004;93:204-8. [Crossref] [PubMed]
- Karlsson S, Varpula M, Ruokonen E, et al. Incidence, treatment, and outcome of severe sepsis in ICU-treated adults in Finland: the Finnsepsis study. Intensive Care Med 2007;33:435-43. [Crossref] [PubMed]
- Sartelli M, Catena F, Ansaloni L, et al. Complicated intra-abdominal infections worldwide: the definitive data of the CIAOW Study. World J Emerg Surg 2014;9:37. [Crossref] [PubMed]
- Leppäniemi A, Kimball EJ, De Laet I, et al. Management of abdominal sepsis - a paradigm shift? Anaesthesiol Intensive Ther 2015;47:400-8. [Crossref] [PubMed]
- Moses ZB, Mayer RR, Strickland BA, et al. Neuronavigation in minimally invasive spine surgery. Neurosurg Focus 2013;35:E12. [Crossref] [PubMed]
- Udby PM, Bech-Azeddine R. Clinical outcome of stand-alone ALIF compared to posterior instrumentation for degenerative disc disease: A pilot study and a literature review. Clin Neurol Neurosurg 2015;133:64-9. [Crossref] [PubMed]
- Wong AP, Smith ZA, Nixon AT, et al. Intraoperative and perioperative complications in minimally invasive transforaminal lumbar interbody fusion: a review of 513 patients. J Neurosurg Spine 2015;22:487-95. [Crossref] [PubMed]
- Fleege C, Rickert M, Rauschmann M. The PLIF and TLIF techniques. Indication, technique, advantages, and disadvantages. Orthopade 2015;44:114-23. [Crossref] [PubMed]
- Lammli J, Whitaker MC, Moskowitz A, et al. Stand-alone anterior lumbar interbody fusion for degenerative disc disease of the lumbar spine: results with a 2-year follow-up. Spine (Phila Pa 1976) 2014;39:E894-901. [Crossref] [PubMed]
- Arnold PM, Anderson KK, McGuire RA Jr. The lateral transpsoas approach to the lumbar and thoracic spine: A review. Surg Neurol Int 2012;3:S198-215. [Crossref] [PubMed]
- Balsano M, Carlucci S, Ose M, et al. A case report of a rare complication of bowel perforation in extreme lateral interbody fusion. Eur Spine J 2015;24 Suppl 3:405-8. [Crossref] [PubMed]
- Bianchi C, Ballard JL, Abou-Zamzam AM, et al. Anterior retroperitoneal lumbosacral spine exposure: operative technique and results. Ann Vasc Surg 2003;17:137-42. [Crossref] [PubMed]
- Birkeland IW Jr, Taylor TK. Bowel injuries coincident to lumbar disk surgery: a report of four cases and a review of the literature. J Trauma 1970;10:163-8. [Crossref] [PubMed]
- Bohinski RJ, Jain VV, Tobler WD. Presacral retroperitoneal approach to axial lumbar interbody fusion: a new, minimally invasive technique at L5-S1: Clinical outcomes, complications, and fusion rates in 50 patients at 1-year follow-up. SAS J 2010;4:54-62. [Crossref] [PubMed]
- Botolin S, Agudelo J, Dwyer A, et al. High rectal injury during trans-1 axial lumbar interbody fusion L5-S1 fixation: a case report. Spine (Phila Pa 1976) 2010;35:E144-8. [Crossref] [PubMed]
- Cakmak A, Gyedu A, Kepenekci I, et al. Colon perforation caused by migration of a bone graft following a posterior lumbosacral interbody fusion operation: case report. Spine (Phila Pa 1976) 2010;35:E84-5. [Crossref] [PubMed]
- Cases-Baldó MJ, Soria-Aledo V, Miguel-Perello JA, et al. Unnoticed small bowel perforation as a complication of lumbar discectomy. Spine J 2011;11:e5-8. [Crossref] [PubMed]
- Goodkin R, Laska LL. Vascular and visceral injuries associated with lumbar disc surgery: medicolegal implications. Surg Neurol 1998;49:358-70; discussion 370-2. [Crossref] [PubMed]
- Hoff-Olsen P, Wiberg J. Small bowel perforation as a complication of microsurgical lumbar diskectomy. A case report and brief review of the literature. Am J Forensic Med Pathol 2001;22:319-21. [Crossref] [PubMed]
- Houten JK, Frempong-Boadu AK, Arkovitz MS. Bowel injury as a complication of microdiscectomy: case report and literature review. J Spinal Disord Tech 2004;17:248-50. [Crossref] [PubMed]
- Keerthi I, Dhillon CS, Shetty MB. Late-onset bowel perforation and iliac artery erosion after prominent anterior spinal instrumentation. Spine (Phila Pa 1976) 2012;37:E1402-5. [Crossref] [PubMed]
- Kim DS, Lee JK, Moon KS, et al. Small bowel injury as a complication of lumbar microdiscectomy: case report and literature review. J Korean Neurosurg Soc 2010;47:224-7. [Crossref] [PubMed]
- Lindley EM, McCullough MA, Burger EL, et al. Complications of axial lumbar interbody fusion. J Neurosurg Spine 2011;15:273-9. [Crossref] [PubMed]
- Mazur MD, Duhon BS, Schmidt MH, et al. Rectal perforation after AxiaLIF instrumentation: case report and review of the literature. Spine J 2013;13:e29-34. [Crossref] [PubMed]
- Nguyen H, Tomita S, Gillingham B. Small bowel perforation from unit rod posterior spinal fusion. J Pediatr Surg 2005;40:e7-8. [Crossref] [PubMed]
- Pappas CT, Harrington T, Sonntag VK. Outcome Analysis in 654 Surgically Treated Lumbar Disc Herniations. Neurosurgery 1992;30:862-6. [PubMed]
- Ruf M, Voigt A, Kupczyk-Joeris D, et al. Perforation of the sigmoid colon due to intradiscal spacer dislocation. Eur Spine J 2011;20 Suppl 2:S289-93. [Crossref] [PubMed]
- Schwartz AM, Brodkey JS. Bowel perforation following microsurgical lumbar discectomy. A case report. Spine (Phila Pa 1976) 1989;14:104-6. [Crossref] [PubMed]
- Shakir AJ, Paterson HM. Small bowel perforation--an unusual complication of microdiscectomy: a case report. Acta Chir Belg 2011;111:36-7. [Crossref] [PubMed]
- Shaw ED, Scarborough JT, Beals RK. Bowel injury as a complication of lumbar discectomy. A case report and review of the literature. J Bone Joint Surg Am 1981;63:478-80. [Crossref] [PubMed]
- Smith EB, DeBord JR, Hanigan WC. Intestinal injury after lumbar discectomy. Surg Gynecol Obstet 1991;173:22-4. [PubMed]
- Smith RA, Estridge MN. Bowel Perforation Following Lumbar-Disc Surgery. Report of a Case with a Review of the Literature. J Bone Joint Surg Am 1964;46:826-8. [Crossref] [PubMed]
- Wilson JR, Timothy J, Rao A, et al. Retrieval of a migrated AxiaLIF lumbosacral screw using fluoroscopic guidance with simultaneous real-time sigmoidoscopy: technical report. Spine (Phila Pa 1976) 2013;38:E1285-7. [Crossref] [PubMed]
- Zileli M, Hoscoskun C, Brastianos P, et al. Surgical treatment of primary sacral tumors: complications associated with sacrectomy. Neurosurg Focus 2003;15:E9. [Crossref] [PubMed]
- Oppenheim H, Krause F. Über einklemmung bzw: strangulation der cauda equina. Dtsch Med Wschr 1909;35:697-700. [Crossref]
- Khoo LT, Ozer AF, Cosar M, et al. History of Minimally Invasive Spine Surgery. In: Minimally Invasive Procedures In Spine Surgery (e-book). Chapter 1, 2016:1.
- Smith L, Garvin PJ, Gesler RM, et al. Enzyme dissolution of the nucleus pulposus. Nature 1963;198:1311-2. [Crossref] [PubMed]
- Hijikata S, Yamagishi M, Nakayama T, et al. Percutaneous discectomy: a new treatment method for lumbar disc herniation. J Toden Hosp 1975;39:5-13.
- Kambin P, Zhou L. History and current status of percutaneous arthroscopic disc surgery. Spine (Phila Pa 1976) 1996;21:57S-61S. [Crossref] [PubMed]
- Kambin P, Zhou L. Arthroscopic discectomy of the lumbar spine. Clin Orthop Relat Res 1997.49-57. [Crossref] [PubMed]
- Forst R, Hausmann B. Nucleoscopy--a new examination technique. Arch Orthop Trauma Surg 1983;101:219-21. [Crossref] [PubMed]
- Cloward RB. The treatment of ruptured lumbar intervertebral discs by vertebral body fusion. I. Indications, operative technique, after care. J Neurosurg 1953;10:154-68. [Crossref] [PubMed]
- Sacks S. Anterior Interbody Fusion of the Lumbar Spine. J Bone Joint Surg Br 1965;47:211-23. [Crossref] [PubMed]
- McAfee PC, Regan JJ, Geis WP, et al. Minimally invasive anterior retroperitoneal approach to the lumbar spine. Emphasis on the lateral BAK. Spine (Phila Pa 1976) 1998;23:1476-84. [Crossref] [PubMed]
- Pimenta L, Diaz RC, Guerrero LG. Charite lumbar artificial disc retrieval: use of a lateral minimally invasive technique. Technical note. J Neurosurg Spine 2006;5:556-61. [Crossref] [PubMed]
- Uribe JS, Deukmedjian AR. Visceral, vascular, and wound complications following over 13,000 lateral interbody fusions: a survey study and literature review. Eur Spine J 2015;24 Suppl 3:386-96. [Crossref] [PubMed]
- Balak N, Demirkesen O, Efendioglu M, et al. Diagnostic approach to reveal retroperitoneal injury during lumbar discectomy. J Neurosurg Sci 2010;54:129-33. [PubMed]
- Bolesta MJ. Vascular injury during lumbar diskectomy associated with peridiskal fibrosis: case report and literature review. J Spinal Disord 1995;8:224-7. [Crossref] [PubMed]
- Harbison SP. Major vascular complications of intervertebral disc surgery. Ann Surg 1954;140:342-8. [Crossref] [PubMed]
- Hadjipavlou A, Alpantaki K, Katonis P, et al. Safety and effectiveness of retrorectal presacral approach for lumbosacral axial instrumentation. A clinical study. Acta Orthop Belg 2013;79:222-9. [PubMed]
- Leavens ME, Bradford FK. Ruptured intervertebral disc; report of a case with a defect in the anterior annulus fibrosus. J Neurosurg 1953;10:544-6. [Crossref] [PubMed]
- Uribe JS, Arredondo N, Dakwar E, et al. Defining the safe working zones using the minimally invasive lateral retroperitoneal transpsoas approach: an anatomical study. J Neurosurg Spine 2010;13:260-6. [Crossref] [PubMed]
- Anda S, Aakhus S, Skaanes KO, et al. Anterior perforations in lumbar discectomies. A report of four cases of vascular complications and a CT study of the prevertebral lumbar anatomy. Spine (Phila Pa 1976) 1991;16:54-60. [Crossref] [PubMed]
- Kanemura T, Satake K, Yamaguchi H, et al. Possibility of colonic perforation during Extreme Lateral Interbody Fusion: Distance between descending or ascending colon and lateral approach pathway. Proceedings of the 9th Annual SOLAS Research Meeting 2016:16-7.


