Perioperative care for lumbar microdiscectomy: a survey of Australasian neurosurgeons
Introduction
Lumbar microdiscectomy is the most commonly performed spine surgery procedure with over 300,000 operations performed annually in the United States alone (1).
The first lumbar discectomy for a patient with a pre-operative diagnosis of ruptured intervertebral disk is credited to Mixter and Barr in 1932 and was performed via a multi-level lumbar laminectomy (2). Since the initial description of the lumbar discectomy procedure the operation has progressed towards its current minimally invasive form. In tandem with the reduction in invasiveness, some surgeons have reduced the restrictions imposed in post-operative care instructions (3). However, significant heterogeneity in surgical technique and perioperative care still exists around the world (4-7) and there is a paucity of literature about the current state of play in Australia.
Understanding current practices would be helpful to patients together with care providers, including referring practitioners, nursing staff, physiotherapists and perhaps other surgeons. The purpose of this survey is to determine current lumbar microdiscectomy perioperative practices amongst Australasian neurosurgeons.
Methods
A survey of Australasian Neurosurgeons was conducted by email invitation sent to all full members of the Neurosurgical Society of Australasia (NSA). All invitees received a further two email reminders. The survey consisted of 11 multi-choice questions conducted by an anonymized online survey. Statistical analysis was performed with Prism 7.0 (GraphPad Software Inc., La Jolla, CA, USA) and SPSS Statistics Version 24 (IBM Corp., Amonk, NY, USA). Pearson chi-squared statistic was used to assess the statistical significance of relationships between surgeon seniority and response to variables. Ethics approval was provided by Monash Human Research Ethics Committee.
Results
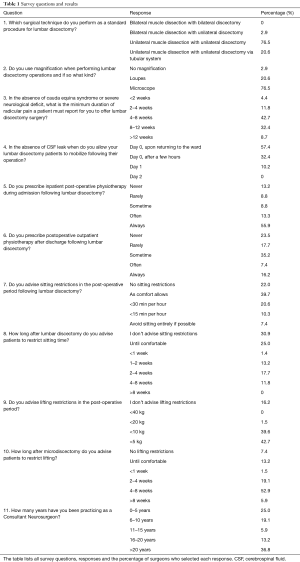
The survey was sent to 235 Australasian Neurosurgeons (NSA Members). Seventy-one responses were received of which 68 were complete (28.9% complete response rate). Only complete responses were included in the attached report. The questions and results of the survey are detailed below in Table 1.
Full table
Surgical procedure
The majority of surgeons (97.1%) performed a unilateral approach; 76.5% of surgeons used a microdiscectomy retractor and 20.6% used a tubular retractor system to perform a unilateral muscle dissection with unilateral discectomy. Only 2.9% of respondents performed bilateral muscle dissection with unilateral discectomy.
Magnification
The operative microscope was the most commonly employed method of magnification, practiced by 76.5% of surgeons. The operative microscope was used by surgeons performing the unilateral muscle dissection technique with a microdiscectomy retractor (58.8%) and those utilizing a tubular retractor system (17.6%). Loupes were used by 20.6% of surgeons—16.2% using the unilateral approach with microdiscectomy retractor, 2.9% using the tubular retractor system and 1.5% using the bilateral muscle dissection approach. Only 2.9% of surgeons elected to use no magnification and these were evenly split between the bilateral and unilateral muscle dissection approach.
Operative indications
In the absence of cauda equina syndrome or severe neurological deficit most surgeons reported that they would consider a period of either 4 to 8 weeks (42.7%) or 8 to 12 weeks (32.4%) of radicular pain the minimum duration of symptoms before offering surgery. Of the remaining surgeons 4.4% considered less than 2 weeks appropriate, 11.8% reported 2 to 4 weeks and 8.7% deemed more than 12 weeks an acceptable period of radicular pain after which surgery could be offered.
Post-operative management
The majority of surgeons (57.4%) mobilized patients upon returning to the ward on the day of surgery. Slightly less than one third of surgeons (32.4%) mobilized patients a few hours after surgery with the remainder (10.2%) mobilizing patients on day 1 following operation.
Post-operative physiotherapy
Most surgeons (55.9%) always referred patients to inpatient physiotherapy. Only 13.2% of surgeons stated they never referred patients to undergo inpatient physiotherapy. Outpatient physiotherapy referral practices were more varied, with 23.5% of surgeons indicating that they never referred patients for outpatient physiotherapy and 16.2% always referring patients for outpatient physiotherapy. The remaining surgeons fell between these extremes.
Sitting restrictions
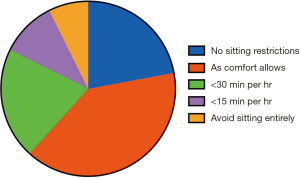
Just over one third of surgeons (38.3%) recommended the application of sitting restrictions whilst the remainder (61.7%) recommended no restrictions beyond that afforded by comfort. The breakdown of this advice can be seen in Table 1 and Figure 1.
When sitting restrictions were recommended the duration varied between avoiding sitting until comfortable (25.0%) and 4 to 8 weeks (11.8%). Sitting restrictions of 2 to 4 weeks were advised by 17.7% of surgeons. Restrictions of 1 week or less were rarely recommended (1.4%).
Lifting restrictions
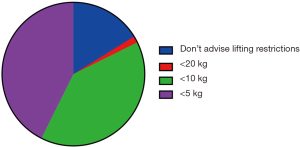
Lifting restrictions were advised by the majority of surgeons (83.8%). Lifting restrictions of <5 kg (42.7%) and <10 kg (39.6%) were most frequently offered. No lifting restrictions were recommended by 16.2% of surgeons (Figure 2). One surgeon contacted the authors directly to stress the importance of the avoidance of spinal flexion rather than lifting per se.
A majority of surgeons advised patients to follow lifting restrictions for a period of 4 to 8 weeks (52.9%). The next most common period was 2 to 4 weeks (19.1%). The application of restrictions until comfortable was advised by 13.2% of surgeons and no period of lifting restrictions advised by 7.4%. A minority of surgeons advised extension of lifting restrictions beyond 8 weeks (5.9%) or for less than 1 week (1.5%).
Seniority and relationship to advising restrictions
There was a representative range of surgeon experience in this study, with surgeons of less than 5 years (25.0% of respondents) to more than 20 years of experience (36.8% of respondents) contributing to the survey. Surgeons 5 years or less post fellowship were more likely to use the operative microscope (94.1%) than those 6 or more years post fellowship (69.2%). The only surgeons who did not use intraoperative magnification had more than 20 years’ experience post fellowship. No relationship between surgical seniority and any other variable achieved statistical significance.
Discussion
This is the first survey of Australasian neurosurgeons detailing the peri-operative management of patients undergoing lumbar discectomy. Australasian practice is generally consistent with international practice and demonstrates a similar degree of heterogeneity (4-7).
A limitation of this study is the 28.9% complete response rate. A trend towards declining responses to clinician surveys has been noted previously (8,9). Reasons cited for this trend include clinicians being “swamped by questionnaires” (10), a lack of incentive for involvement (10) and many clinicians having a policy of non-response (9). Furthermore Australasian clinicians have been noted to be amongst the worst survey responders (8). The response rate is comparable to the 36% rate in a survey of members of the International Society for the Study of the Lumbar Spine regarding post-operative activity restrictions (11). The distribution of surgeon seniority in this survey approximates that of the neurosurgical workforce as described in the 2016 Royal Australasian College of Surgeons Activities Report suggesting that responders are representative in this regard (12). The potential for non-responder bias must, however, be recognized.
Unilateral muscle dissection with unilateral discectomy is the approach taken by the majority of Australasian neurosurgeons and is consistent with the reported practices of Dutch spine surgeons (4). The nature of the operative approach preferred by British, Canadian and Italian surgeons was not reported.
Concurrent with the trend towards reduced soft tissue dissection in lumbar discectomy increased use of operative magnification has also been practiced (13). The operating microscope was introduced to lumbar discectomy surgery by Yasargil in 1967 and reported as part of a series of patients in 1977 (14). Its use was subsequently popularized by the pioneering orthopedic spine surgeon John McCulloch (13,15) and is the practice of over three quarters of Australasian neurosurgeons surveyed. Canadian neurosurgeons reported a similar practice with 70% using the microscope (5). Similarly, 82.5% of neurosurgeons from Lombardy reported using either loupes or the operative microscope (the two were not distinguished in the Italian survey) while 17.5% reported no use of magnification, much higher than the 3% in our survey. The figures for Dutch and British surgeons were not reported.
Variation among spine surgeons regarding timing of surgery in patients with radicular pain has been noted in previous studies (4). The majority of Australasian neurosurgeons surveyed consider a period of 4 to 8 weeks (42.65%) or 8 to 12 weeks (32.35%) the minimum period of radicular pain a patient must report prior to being offered lumbar discectomy surgery in the absence of cauda equina syndrome. These figures are very similar to those reported by Dutch spine surgeons—34% of surgeons indicated they would offer surgery to patients with 4 to 8 weeks of symptoms and a further 42% would offer surgery at 8 to 12 weeks (4).
Timing of surgery for lumbar disk herniation associated sciatica is a long-standing controversy amongst spine surgeons. Surgical practice has swung from periods of early surgical intervention for acute radicular pain (16) to the current approach favored by most surgeons of performing a trial of conservative management lasting a number of weeks. The evidence from randomized controlled trials suggests early surgical intervention may offer symptomatic benefit. On as-treated analysis, the Spine Patient Outcomes Research Trial (SPORT) (17,18), demonstrated statistically significant benefits to surgery at all time-points from 3 months to 4 years (17,18). Similarly, the Sciatica Trial, comparing early (6 to 14 weeks) surgery for sciatica with 6 months of conservative management and surgery thereafter if required, demonstrated faster pain relief and perceived recovery in those who received early surgery (19).
Just over half of Australian neurosurgeons always prescribe post-operative inpatient physiotherapy with less, only 1 in 6, always prescribing outpatient physiotherapy. International practice regarding physiotherapy referral varied significantly: 85.7% of Dutch surgeons prescribed inpatient physiotherapy while only 6% of Italian neurosurgeons did the same. This reflects the lack of clarity regarding the role of post-operative physiotherapy following lumbar microdiscectomy. A recent Cochrane review of post-operative rehabilitation programs following lumbar microdiscectomy indicated that there is, at best, low level evidence that physiotherapy programs started 4 to 6 weeks post-surgery led to better function than no treatment (20).
Post-operative activity restrictions are commonly imposed following lumbar discectomy. This can be observed in our survey and a survey of international surgeons specifically addressing lifting restrictions following spine surgery (11). Our survey results reflect the persistence of this practice with approximately 40% of Australasian neurosurgeons recommending specific sitting restrictions. A survey of British spine surgeons indicated that 31% request their patients do not sit for between 2 days to 6 weeks following a spine surgical procedure (6). The British survey does not provide further detail on sitting restrictions and data for post-operative sitting restrictions were not available for Dutch, Italian or Canadian spine surgeons.
Lifting restrictions were more common, with specific lifting restrictions advised by the majority of Australasian neurosurgeons (83.2%). Approximately half of Australasian neurosurgeons advised the application of such restrictions for a period of 4 to 8 weeks. The recommendation for lifting restrictions is relatively consistent with the practice among British spine surgeons and surgeons of the International Society for the Study of Lumbar Spine Surgery, 85% (6) and 96.3% (11) of whom respectively advised lifting restrictions (6). The variety of lifting restrictions demonstrated in this survey are consistent with earlier reports of European spine surgeon recommendations in which the authors noted a lack of consistency (11).
The underlying rationale for sitting and lifting restrictions is that following surgery the spine is weaker due to disruption of the functional spinal motion unit and thus potentially more prone to injury (11). However, there appears to be little evidence to support this theory, empirically or biomechanically, or the imposition of such restrictions (11,21). The purpose of such restrictions in the era of microdiscectomy has been questioned in the literature since at least the mid-1990s (3,22). Carragee et al. reported a prospective study of 152 patients who did not observe activity restrictions following lumbar microdiscectomy. This cohort achieved similar outcomes, with the exception of achieving earlier return to work, compared to literature reported outcomes for the standard practice of post-operative restrictions. Bono et al. (23) recently reported the first randomized controlled trial comparing post-operative activity restriction protocols following lumbar microdiscectomy. No significant differences in outcomes or disk herniation recurrence rates were observed with activity restriction protocols of 2 or 6 weeks. The study was, however, underpowered to detect a significant difference in reherniation rates. We are currently performing the first randomized controlled trial comparing a patient group observing no post-operative activity restrictions with a control group observing a one month period of activity restrictions (24). Additionally, our study will track patient adherence to activity restrictions following spine surgery through use of a wearable activity monitory, an innovation of importance given the difficulty of verifying patient adherence to activity restrictions through self-report.
Conclusions
In conclusion, the surgical techniques and magnification preference of Australian neurosurgeons are generally consistent with their international colleagues. Sitting and lifting restrictions are still frequently advised by Australasian neurosurgeons. This survey demonstrates the heterogeneity in peri-operative practices of Australasian neurosurgeons and suggests the potential for investigation of the role of post-operative activity restrictions following lumbar microdiscectomy given the prevalence and variety of these practices in the era of minimally invasive spine surgery.
Acknowledgements
Dr. CD Daly is the recipient of the Foundation for Surgery Richard Jepson Research Scholarship. The authors thank the Neurosurgical Society of Australasia and its members for their participation and contribution to this report.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethics approval was provided by Monash Human Research Ethics Committee (No. 15379L).
References
- Parker SL, Xu R, McGirt MJ, et al. Long-term back pain after a single-level diskectomy for radiculopathy: incidence and health care cost analysis. J Neurosurg Spine 2010;12:178-82. [Crossref] [PubMed]
- Mixter WJ, Barr JS. Rupture of the intervertebral disk with involvement of the spinal canal. N Engl J Med 1934;211:210-4. [Crossref]
- Carragee EJ, Helms E, O'Sullivan GS. Are postoperative activity restrictions necessary after posterior lumbar diskectomy? A prospective study of outcomes in 50 consecutive cases. Spine (Phila Pa 1976) 1996;21:1893-7. [Crossref] [PubMed]
- Arts MP, Peul WC, Koes BW, et al. Management of sciatica due to lumbar disk herniation in the Netherlands: a survey among spine surgeons. J Neurosurg Spine 2008;9:32-9. [Crossref] [PubMed]
- Cenic A, Kachur E. Lumbar diskectomy: a national survey of neurosurgeons and literature review. Can J Neurol Sci 2009;36:196-200. [Crossref] [PubMed]
- McGregor AH, Dicken B, Jamrozik K. National audit of post-operative management in spinal surgery. BMC Musculoskelet Disord 2006;7:47. [Crossref] [PubMed]
- Zoia C, Bongetta D, Poli JC, et al. Intraregional differences of perioperative management strategy for lumbar disk herniation: is the Devil really in the details? Int J Spine Surg 2017;11:1. [Crossref] [PubMed]
- Cook JV, Dickinson HO, Eccles MP. Response rates in postal surveys of healthcare professionals between 1996 and 2005: An observational study. BMC Health Serv Res 2009;9:160. [Crossref] [PubMed]
- Wiebe ER, Kaczorowski J, MacKay J. Why are response rates in clinician surveys declining? Can Fam Physician 2012;58:e225-8. [PubMed]
- McAvoy BR, Kaner EF. General practice postal surveys: a questionnaire too far? BMJ 1996;313:732-3; discussion 733-4. [Crossref] [PubMed]
- Magnusson ML, Pope MH, Wilder DG, et al. Is there a rational basis for post-surgical lifting restrictions? 1. Current understanding. Eur Spine J 1999;8:170-8. [Crossref] [PubMed]
- RACS. Royal Australasian College of Surgeons 2016 Annual Activities Report. 2017:41-2.
- Truumees E. A history of lumbar disk herniation from Hippocrates to the 1990s. Clin Orthop Relat Res 2015;473:1885-95. [Crossref] [PubMed]
- Yasargil MG. Microsurgical Operation of Herniated Lumbar Disk. In: Wüllenweber R, Brock M, Hamer J, et al. editors. Lumbar Disk Adult Hydrocephalus. Berlin: Springer, 1977:81.
- McCulloch JA. Focus issue on lumbar disk herniation: macro- and microdiskectomy. Spine (Phila Pa 1976) 1996;21:45S-56S. [Crossref] [PubMed]
- Postacchini F, Postacchini R. Operative management of lumbar disc herniation: the evolution of knowledge and surgical techniques in the last century. Acta Neurochir Suppl 2011;108:17-21. [Crossref] [PubMed]
- Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA 2006;296:2441-50. [Crossref] [PubMed]
- Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonoperative treatment for lumbar disc herniation: four-year results for the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976) 2008;33:2789-800. [Crossref] [PubMed]
- Peul WC, van Houwelingen HC, van den Hout WB, et al. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med 2007;356:2245-56. [Crossref] [PubMed]
- Oosterhuis T, Costa LO, Maher CG, et al. Rehabilitation after lumbar disk surgery. Cochrane Database Syst Rev 2014.CD003007. [PubMed]
- Pope MH, Magnusson ML, Wilder DG, et al. Is there a rational basis for post-surgical lifting restrictions? 2. Possible scientific approach. Eur Spine J 1999;8:179-86. [Crossref] [PubMed]
- Carragee EJ, Han MY, Yang B, et al. Activity restrictions after posterior lumbar diskectomy. A prospective study of outcomes in 152 cases with no postoperative restrictions. Spine (Phila Pa 1976) 1999;24:2346-51. [Crossref] [PubMed]
- Bono CM, Leonard DA, Cha TD, et al. The effect of short (2-weeks) versus long (6-weeks) post-operative restrictions following lumbar diskectomy: a prospective randomized control trial. Eur Spine J 2017;26:905-12. [Crossref] [PubMed]
- Daly CD, Lim KZ, Lewis J, et al. Lumbar microdiscectomy and post-operative activity restrictions: a protocol for a single blinded randomised controlled trial. BMC Musculoskelet Disord 2017;18:312. [Crossref] [PubMed]