C7 intra-laminar screws for complex cervicothoracic spine surgery—a case series
Introduction
The cervicothoracic junction provides a similar yet different challenge to the thoracolumbar junction in that it marks the transition from the mobile cervical spine to the relatively rigid thoracic spine, yet the anatomy of the cervical and lumbar vertebrae is markedly contrasted. In contrast to the thoracolumbar junction, the mainstay of posterior fixation in the subaxial cervical spine is lateral mass fixation with high fusion and low complication rates (1), compared to similar results obtained with thoracic pedicle screw fixation (2-4). Of note, C7 has been successfully used as an anchor point using its lateral masses (5) and pedicles (6,7), although in many patients the lateral mass of C7 may be small, and pedicle fixation can be technically demanding and require a wide exposure. Higher level cervical pedicle screw fixation has been well described but is also technically challenging with greater consequences of pedicle breaches (8).
Similar to the thoracolumbar junction, pathology requiring fixation in the cervicothoracic junction is variable. An et al. reported a diverse range of pathologies involving the cervicothoracic junction in 36 patients (9), and in one series of cervical spinal trauma, 9% involved the cervicothoracic junction (10).
One of the additional challenges of transitioning from lateral mass screws in the cervical spine to pedicle screws in the upper thoracic spine is appropriate rod contouring. Notching of rods has been shown to reduce the strength of implanted rods, and so any construct that minimizes this can potentially reduce the chance of fatigue cracking (11,12).
Bozkus et al. showed that posterior fixation alone is stronger than anterior alone instrumentation in 2 level lower cervical instrumentation, with combined approaches providing increased rigidity. They also noted that there was no difference between pure pedicle cervical pedicle screw fixation and combined lateral mass/pedicle screw fixation (13). The increased rigidity of posterior fixation compared to anterior plating was also confirmed by Bueff et al. (14).
The C7 laminar is a relatively novel posterior fixation point, but has been used safely and effectively at our institution. The purpose of this study was to review the outcomes of our cases where C7 laminar fixation was used.
Methods
Retrospective data was analysed using following Institute Review Board (IRB) approval as part of the Spine Tango database at our institution. Spine Tango data and medical records of all patients treated by the primary surgeon (MS) from February 2013 to July 2016 were reviewed.
The surgical technique is similar to the well described technique for C2 laminar screw fixation as described by Wright (15). Pre-operative computed tomograms (CT) or magnetic resonance imaging (MRI) scans are measured to determine if 3.5 mm screws can be safely placed within the cortical margins of the C7 laminar. Open exposure of the C7 laminar is made with preservation, if appropriate and possible, of muscular attachments at the tip of the spinous process. A high speed drill or pedicle awl is used to enter on the laminar margin, often at the junction with the spinous process, and the contralateral laminar visualized to determine appropriate angle and height. As the second screw can be more difficult to place, the first screw should be placed slightly higher within the laminar as the C7 laminar is typically thinner superiorly. This allows the second screw to be placed inferiorly in the laminar. Following entry to the cancellous bone of the laminar the pedicle probe or burr is used to advance to a depth of typically 26–34 mm in the contralateral laminar from the starting point. Palpation of the previously probed tract using a pedicle sound/feeler is used to confirm integrity of the laminar walls and then tapping is performed prior to definitive screw placement. Polyaxial 3.5 mm fully threaded screws, usually used for pedicle or lateral mass fixation, should be left 1–2 mm proud of the entry point to allow for rod connection. The screws form a crossing inter-laminar construct.
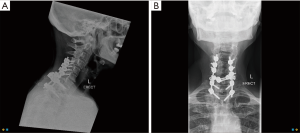
In the case of C7 laminar screws being used in a long cervicothoracic construct, short trans-connectors are recommended to attach the screws to the rods, allowing a smooth transition between C6 lateral mass screws and T1 pedicle screws. A cut 3.5 mm crosslink is an alternative to trans-connectors (Figure 1A,B).
Results
Ten patients had C7 laminar screws sited. Nine patients had bilateral C7 laminar screws and one patient had a unilateral C7 laminar screw sited. Six patients had trauma as an underlying pathology and all had anterior fixation which was augmented by posterior fixation, 2 of which were related to pseudoarthrosis from previous anterior stand-alone surgery. Two degenerative cases for cervicothoracic deformity with myelopathy involved combined staged anterior and posterior instrumentation, correction of deformity and fusion. One degenerative and one tumour case (pathological fracture) required posterior fixation alone. There were 6 males and 4 females. Median follow up was 1 year for all surviving patients (range: 6 months to 4 years). All patients undergoing fusions for degenerative conditions had greater than 1 year clinical and radiological follow-up. The single patient with only 6 months follow-up underwent surgery for an unstable fracture of the ankylosed spine and is the last patient in the reported cohort.
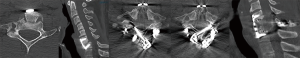
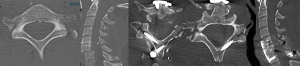
No intra-operative complications were identified and all screws were contained entirely within the laminar in the nine patients with post-operative CT imaging. The remaining patient passed away 2 weeks post-operatively due to respiratory failure from a cervical spinal cord injury, prior to standard post-operative CT being performed.
One patient with a pathological fracture secondary to multiple metastasis and spinal cord compression died 6 months following surgery secondary to progression of extra-spinal disease. One patient with degenerative disease was a revision case and had superficial wound breakdown without infection requiring debridement.
One patient required removal of crossing C7 laminar screws for a posterior laminectomy and intra-dural surgery after solid fusion was achieved due to a cerebrospinal fluid (CSF) circulation disorder with syrinx formation. This was at the site of a traumatic spinal cord injury secondary to a fracture of the ankylosed spine. CT scan prior to removal showed complete fracture healing with well-placed C7 laminar screws. At the time of surgical removal, a solid arthrodesis was confirmed and the screws, end caps and associated short transconnectors removed easily from the middle of the construct without complication.
All surviving patients had clinical and radiological evidence of complete fracture healing or solid arthrodesis at last follow-up with no evidence of instrumentation failure.
Figures 2 and 3 show the pre- and post-operative key CT images in two of the patients who successfully underwent C7 laminar fixation following anterior stabilization in the setting of trauma.
Discussion
Feasibility of the C7 laminar as a fixation point was first reported in a cadaveric study by Cao et al. and found that 16 of their 22 cadavers studied had a laminar thickness of at least 4.5 mm. Jang et al. reviewed 120 CT scans and found that 239 of 240 C7 laminae would be suitable for a 3.5 mm screw with 1 mm clearance on either side (16). A biomechanical comparison by Hong et al. (17) showed equivalent pullout strength of C7 laminar screws and C7 pedicle screws, both being superior to lateral mass fixation, but otherwise superior biomechanics of pedicle screw fixation. Shin et al. reviewed 215 CT scans for 430 C7 laminae and found feasibility for unilateral fixation in 91.4% and bilateral fixation in 68.8%, of note the anatomy being generally more favourable in men than women (18). Alvin et al. reviewed 50 CT scans and found that unilateral laminar screws would be suitable in 100% of cases at C7, and bilateral in 96% of men and 84% of women (19). Lin et al. measured 20 cadaveric spines using CT and digital calipers, and found that all would be suitable for C7 laminar screws (20). Ilgenfritz et al. found in a radiographic study of 72 CT scans and biomechanical study of 13 cadaveric cervical spines that the majority of C7 levels would accept laminar screws based on width, all would accept bilateral screws based on height, and pullout strength was equivalent to C7 pedicle screws and greater than C2 laminar screw fixation (21). Baek et al. performed a cadaveric study on 18 spines and found that when divided into thirds, the upper third would accommodate a 3.5 mm screw in 14/36 (38.9%), the middle third in 32/36 (88.9%), and the lower third in 28/36 (77.8%) (22). A final biomechanical study was also performed by Hong et al. showed superiority of pedicle screw fixation in C7 but with superiority of laminar fixation when compared to the lateral mass (23).
Few case series have previously reported results regarding the C7 laminar as a fixation point. Hong et al. first reported 4 patients with C7 laminar screw fixation, 2 with bilateral screws and 2 with unilateral screws (24). No complications other than one asymptomatic dorsal breach of the laminar were reported. The same 4 patients were then reported in combination with a series of 21 patients with C2 laminar screws (25). Jang et al. described 13 patients with 17 C7 laminar screws, with 2 dorsal breaches and no other complications identified (26). A case report of successful C7 laminar screw to supplement C3–7 lateral mass fixation was made by Koltz et al. (27). Finally, Xia et al. reported a series of 12 patients with unilateral or bilateral C7 laminar screws sited without complication (28).
In analysis of alternative fixation points, namely the C7 pedicle and lateral mass, Xu et al. found the pedicles of C7 to have more consistent anatomy than the lateral masses (29). Abdullah et al. measured the lateral masses of C5, C6 and C7 on the CT scans of 25 males and 25 females, finding that although C7 decreased in medial-to-lateral width compared to other levels, they also had an increase in sagittal height and sagittal diagonal height, with no significant difference in volume of lateral mass between any of the measured levels (30). Ebraheim et al. assessed nerve root position relative to the superior articular facets for the C3 to C7 lateral masses, and found the C7 root was closest to the superior articular facet (mean distance 8.5 mm +/−0.9) (31). Mazel et al. reported 32 patients who underwent posterior fixation for cervicothoracic junction tumours, and identified two patients where the C7 lateral mass screws crossed the articular facet, but managed to avoid injuring the C8 nerve root. They attributed the use of short screws as an explanation for avoidance of this complication, although they did state a preference for bicortical fixation at that level (32).
Tatsumi et al. compared mechanical parameters of four different rod-and-screw-based constructs for crossing the cervicothoracic junction. The weakest of construct involved paired 3.5 mm diameter rods, which was shown to be inferior to paired 3.5 mm/5.5 mm transitional rods, as well as paired 3.5 and 5.5 mm rods joined with solid or hinged domino connectors (33). However, Yang et al. showed increased complication rates, blood loss and operating time associated with transitional rods over small rods, with nonetheless similar pseudoarthrosis rates (34). A biomechanical study simulating C7/T1 injury used lateral mass screw fixation in C5 and C6, with pedicle screw fixation in T1 and T2 with two rod-screw systems and one plate-screw system showed satisfactory stabilization with all three constructs for a two-column injury, but not for a three-column injury without anterior stabilization (35). To our knowledge there is no biomechanical study of a rod construct involving C7 laminar fixation; this would worth performing in the future to confirm adequacy of using C7 laminar fixation in posterior constructs.
Conclusions
Use of the C7 laminar as fixation point in constructs that cross or stop at the cervicothoracic junction allows for ease of rod placement with minimisation of rod contouring without compromising biomechanical stability. Further, larger case series and biomechanical testing is warranted to confirm its clinical utility.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Retrospective data was analysed using following Institute Review Board (IRB) approval as part of the Spine Tango database at our institution. Spine Tango data and medical records of all patients treated by the primary surgeon (MS) from February 2013 to July 2016 were reviewed.
References
- Coe JD, Vaccaro AR, Dailey AT, et al. Lateral mass screw fixation in the cervical spine: a systematic literature review. J Bone Joint Surg Am 2013;95:2136-43. [Crossref] [PubMed]
- Schizas C, Theumann N, Kosmopoulos V. Inserting pedicle screws in the upper thoracic spine without the use of fluoroscopy or image guidance. Is it safe? Eur Spine J 2007;16:625-9. [Crossref] [PubMed]
- Daubs MD, Kim YJ, Lenke LG. Pedicle screw fixation (T1, T2, and T3). Instr Course Lect 2007;56:247-55. [PubMed]
- Avila MJ, Baaj AA. Freehand Thoracic Pedicle Screw Placement: Review of Existing Strategies and a Step-by-Step Guide Using Uniform Landmarks for All Levels. Cureus 2016;8:e501. [PubMed]
- Sekhon LH. Posterior cervical lateral mass screw fixation: analysis of 1026 consecutive screws in 143 patients. J Spinal Disord Tech 2005;18:297-303. [Crossref] [PubMed]
- Cho W, Eid AS, Chang UK. The use of pedicle screw-rod system for the posterior fixation in cervico-thoracic junction. J Korean Neurosurg Soc 2010;48:46-52. [Crossref] [PubMed]
- Liao W, Guo L, Bao H, et al. Morphometric analysis of the seventh cervical vertebra for pedicle screw insertion. Indian J Orthop 2015;49:272-7. [Crossref] [PubMed]
- Ludwig SC, Kramer DL, Balderston RA, et al. Placement of pedicle screws in the human cadaveric cervical spine: comparative accuracy of three techniques. Spine (Phila Pa 1976) 2000;25:1655-67. [Crossref] [PubMed]
- An HS, Vaccaro A, Cotler JM, et al. Spinal disorders at the cervicothoracic junction. Spine (Phila Pa 1976) 1994;19:2557-64. [Crossref] [PubMed]
- Nichols CG, Young DH, Schiller WR. Evaluation of cervicothoracic junction injury. Ann Emerg Med 1987;16:640-2. [Crossref] [PubMed]
- Yamanaka K, Mori M, Yamazaki K, et al. Analysis of the Fracture Mechanism of Ti-6Al-4V Alloy Rods That Failed Clinically After Spinal Instrumentation Surgery. Spine (Phila Pa 1976) 2015;40:E767-73. [Crossref] [PubMed]
- Dick JC, Bourgeault CA. Notch sensitivity of titanium alloy, commercially pure titanium, and stainless steel spinal implants. Spine (Phila Pa 1976) 2001;26:1668-72. [Crossref] [PubMed]
- Bozkus H, Ames CP, Chamberlain RH, et al. Biomechanical analysis of rigid stabilization techniques for three-column injury in the lower cervical spine. Spine (Phila Pa 1976) 2005;30:915-22. [Crossref] [PubMed]
- Bueff HU, Lotz JC, Colliou OK, et al. Instrumentation of the cervicothoracic junction after destabilization. Spine (Phila Pa 1976) 1995;20:1789-92. [Crossref] [PubMed]
- Wright NM. Posterior C2 fixation using bilateral, crossing C2 laminar screws: case series and technical note. J Spinal Disord Tech 2004;17:158-62. [Crossref] [PubMed]
- Jang WY, Kim IS, Lee HJ, et al. A computed tomography-based anatomic comparison of three different types of c7 posterior fixation techniques: pedicle, intralaminar, and lateral mass screws. J Korean Neurosurg Soc 2011;50:166-72. [Crossref] [PubMed]
- Hong JT, Tomoyuki T, Udayakumar R, et al. Biomechanical comparison of three different types of C7 fixation techniques. Spine (Phila Pa 1976) 2011;36:393-8. [Crossref] [PubMed]
- Shin SI, Yeom JS, Kim HJ, et al. The feasibility of laminar screw placement in the subaxial spine: analysis using 215 three-dimensional computed tomography scans and simulation software. Spine J 2012;12:577-84. [Crossref] [PubMed]
- Alvin MD, Abdullah KG, Steinmetz MP, et al. Translaminar screw fixation in the subaxial cervical spine: quantitative laminar analysis and feasibility of unilateral and bilateral translaminar virtual screw placement. Spine (Phila Pa 1976) 2012;37:E745-51. [Crossref] [PubMed]
- Lin HJ, Xu RM, Liu GY, et al. Zhongguo Gu Shang 2012;25:594-8. [Anatomic study of lower cervical spinous process for laminar screw fixation]. [PubMed]
- Ilgenfritz RM, Gandhi AA, Fredericks DC, et al. Considerations for the use of C7 crossing laminar screws in subaxial and cervicothoracic instrumentation. Spine (Phila Pa 1976) 2013;38:E199-204. [Crossref] [PubMed]
- Baek TH, Kim I, Hong JT, et al. Feasibility of bilateral crossing c7 intralaminar screws: a cadaveric study. J Korean Neurosurg Soc 2014;56:5-10. [Crossref] [PubMed]
- Hong JT, Qasim M, Espinoza Orias AA, et al. A biomechanical comparison of three different posterior fixation constructs used for c6-c7 cervical spine immobilization: a finite element study. Neurol Med Chir (Tokyo) 2014;54:727-35. [Crossref] [PubMed]
- Hong JT, Sung JH, Son BC, et al. Significance of laminar screw fixation in the subaxial cervical spine. Spine (Phila Pa 1976) 2008;33:1739-43. [Crossref] [PubMed]
- Hong JT, Yi JS, Kim JT, et al. Clinical and radiologic outcome of laminar screw at C2 and C7 for posterior instrumentation--review of 25 cases and comparison of C2 and C7 intralaminar screw fixation. World Neurosurg 2010;73:112-8; discussion e15.
- Jang SH, Hong JT, Kim IS, et al. C7 posterior fixation using intralaminar screws: early clinical and radiographic outcome. J Korean Neurosurg Soc 2010;48:129-33. [Crossref] [PubMed]
- Koltz MT, Maulucci CM, Sansur CA, et al. C7 intralaminar screw placement, an alternative to lateral mass or pedicle fixation for treatment of cervical spondylytic myelopathy, kyphotic deformity, and trauma: A case report and technical note. Surg Neurol Int 2014;5:4. [Crossref] [PubMed]
- Xia DD, Yan MJ, Zhang JJ, et al. Modified translaminar screw fixation in the cervicothoracic junction (C7-T2): a technical note. Eur Spine J 2016;25:1661-4. [Crossref] [PubMed]
- Xu R, Ebraheim NA, Yeasting R, et al. Anatomy of C7 lateral mass and projection of pedicle axis on its posterior aspect. J Spinal Disord 1995;8:116-20. [Crossref] [PubMed]
- Abdullah KG, Steinmetz MP, Mroz TE. Morphometric and volumetric analysis of the lateral masses of the lower cervical spine. Spine (Phila Pa 1976) 2009;34:1476-9. [Crossref] [PubMed]
- Ebraheim NA, Xu R, Stanescu S, et al. Anatomic relationship of the cervical nerves to the lateral masses. Am J Orthop (Belle Mead NJ) 1999;28:39-42. [PubMed]
- Mazel C, Hoffmann E, Antonietti P, et al. Posterior cervicothoracic instrumentation in spine tumors. Spine (Phila Pa 1976) 2004;29:1246-53. [Crossref] [PubMed]
- Tatsumi RL, Yoo JU, Liu Q, et al. Mechanical comparison of posterior instrumentation constructs for spinal fixation across the cervicothoracic junction. Spine (Phila Pa 1976) 2007;32:1072-6. [Crossref] [PubMed]
- Yang JS, Buchowski JM, Verma V. Construct Type and Risk Factors for Pseudarthrosis at the Cervicothoracic Junction. Spine (Phila Pa 1976) 2015;40:E613-7. [Crossref] [PubMed]
- Kreshak JL, Kim DH, Lindsey DP, et al. Posterior stabilization at the cervicothoracic junction: a biomechanical study. Spine (Phila Pa 1976) 2002;27:2763-70. [Crossref] [PubMed]


