Unusual imaging presentation of spinal glomus tumor: case report
Introduction
The normal glomus body is an arteriovenous anastomosis existed in the dermis layer of skin for thermoregulation (1,2). A glomangioma, also known as a glomus tumor, is a benign lesion and most located in the extremities (3). Reviewing previous publication, all of the primary spinal glomus tumors were demonstrated osteolytic patterns under radiological examination (4-9). In this study, we presented a case with spinal glomus tumor causing myelopathy and a different computed tomography (CT) imaging presentation of reactive sclerotic change.
Case presentation
History
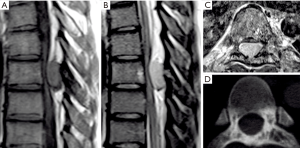
A 26-year-old man presented with progressive paraparesis that had commenced 3 months previously. There were also paresthesia and hyperreflexia in both legs, but no bowel or bladder symptoms. Magnetic resonance images (MRIs) of the thoracic spine demonstrated an enlarged mass, causing spinal cord compression, which had the characteristics of a neuroma or a schwannoma. The tumor had iso-intensity on the T1-weighted MRI (Figure 1A), hyper-intensity on the T2-weighted MRI (Figure 1B) and a strong enhancement on the T1-weighted MRI (Figure 1C). There was reactive sclerotic change which was noticed on the pre-operative CT scans (Figure 1D). Due to progressive weakness and impaired sensation, the patient opted to undergo surgery for resection of the lesion.
Operative findings and outcomes
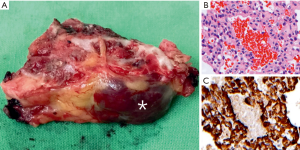
Under general anesthesia, the patient was under prone position with intraoperative C-arm guidance for lesion localization. During the operation, a hypervascular lesion (Figure 2A, marked by an asterisk) beneath the inner cortex of lamina over the same level was removed en bloc. Post operation, the patient’s thoracic myelopathy improved greatly. The pathology report revealed some cavernous haemangioma-like vascular structures surrounded by many small clusters of glomus cells (Figure 2B) with immunoreactive for smooth muscle actin (Figure 2C), and was diagnosed as glomangioma.
Discussion
Glomus tumors were most found in hands, especially fingertips (10). For glomus tumors in hands, the successful rate of surgical excision could be greater than 95% with local recurrence rate of less than 5% for 2-year follow-up (11,12). Extradigital intraosseous glomus tumors are extremely rare. There were few published literatures including the primary or metastatic spinal glomus tumor (4-9,13). In the presenting case, we demonstrated a patient with compressive myelopathy caused by an intraspinal epidural glomus tumor. Unusual reactive sclerotic change was found over body, lamina and pedicle regions. After surgical en bloc resection, the patient had well recovery under uneventful follow-up.
For imaging presentation, Lee et al. (2) reviewed the 11 cases with extradigital glomus tumors over extremity, buttock and scapula regions. Under MRI examination, these lesions were ovoid and well defined, and were illustrated hypointensity or isointensity on T1- and hyperintensity on T2-weighted MRI images. Compared with the intraosseous glomus tumors, there were seven cases (including our presenting case) with the primary spinal lesions. Except some cases without providing MRI information, most of cases were illustrated hyperintensity or isointensity on T2-weighted images, but the presentation of T1-weighted image was not consistent (Table1).

Full table
Under the CT examination, six cases with the primary glomus tumor were published before. Five of them revealed osteolytic pattern on figures illustrated. The rest of one case was also mentioned osteolytic finding during surgery. In our presenting case, there was no osteolytic lesion, but reactive sclerotic change over the body and lamina was found over the same level of the tumor located (Table 1). There is no evidence to explain this finding. However, Kim et al. reviewed 19 consecutive patients with solitary spinal bone lesions found on MRI and CT examination. Compared the final surgical pathological results with different presentations of MRI and CT examinations, the percentage of reactive sclerotic change in the benign lesions was significantly higher than that in the malignant lesion (14).
The glomus tumor was a rare spinal lesion. The previous literature was illustrated different presentation of myelopathy with or without radiculopathy (4-8). In our case, abnormal bone reaction was found on the pre-operative CT scan, unlike the osteolytic pattern of the previous cases published before (5,6,8). The radiological diagnosis was difficult pre-operatively. Surgical resection for definite pathology was suggested.
Conclusions
Preoperatively radiological diagnosis of spinal glomus tumor has limitation. For patient with spinal compressive myelopathy with neurological deficit, surgical intervention was suggested not only for relieving symptoms but confirming pathological diagnosis.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Urakawa H, Nakashima H, Yamada Y, et al. Intraosseous glomus tumor of the ulna: a case report with radiographic findings and a review of the literature. Nagoya J Med Sci 2008;70:127-33. [PubMed]
- Lee S, Le H, Munk P, et al. Glomus tumour in the forearm: a case report and review of MRI findings. JBR-BTR 2010;93:292-5. [PubMed]
- Googe PB, Griffin WC. Intravenous glomus tumor of the forearm. J Cutan Pathol 1993;20:359-63. [Crossref] [PubMed]
- Bessho Y, Kataoka O, Sho T, et al. Intraosseous glomus tumor in the upper thoracic spine complicating compression myelopathy. A case report. Spine (Phila Pa 1976) 1991;16:988-90. [Crossref] [PubMed]
- Robinson JC, Kilpatrick SE, Kelly DL Jr. Intraosseous glomus tumor of the spine. Case report and review of the literature. J Neurosurg 1996;85:344-7. [Crossref] [PubMed]
- Payer M, Grob D, Benini A, et al. Intraosseous glomus tumor of the thoracic spine. Case illustration. J Neurosurg 2002;96:137. [PubMed]
- Bambakidis NC, Gore P, Eschbacher J, et al. Intraosseous spinal glomus tumors: case report. Neurosurgery 2007;60:E1152-3; discussion E1153.
- Becce F, Richarme D, Letovanec I, et al. Percutaneous radiofrequency ablation of primary intraosseous spinal glomus tumor. Skeletal Radiol 2012;41:467-72. [Crossref] [PubMed]
- Liu T, Zou W, Kong J, et al. Embolization in the treatment of an intraosseous glomus tumor in the upper thoracic spine complicating compression myelopathy: a case report and a literature review. Turk Neurosurg 2015;25:479-84. [PubMed]
- Baek HJ, Lee SJ, Cho KH, et al. Subungual tumors: clinicopathologic correlation with US and MR imaging findings. Radiographics 2010;30:1621-36. [Crossref] [PubMed]
- Van Geertruyden J, Lorea P, Goldschmidt D, et al. Glomus tumours of the hand. A retrospective study of 51 cases. J Hand Surg Br 1996;21:257-60. [Crossref] [PubMed]
- Friske JE, Sharma V, Kolpin SA, et al. Extradigital glomus tumor: a rare etiology for wrist soft tissue mass. Radiol Case Rep 2016;11:195-200. [Crossref] [PubMed]
- Nagata K, Hashizume H, Yamada H, et al. Long-term survival case of malignant glomus tumor mimicking "dumbbell-shaped" neurogenic tumor. Eur Spine J 2017;26:42-46. [Crossref] [PubMed]
- Kim YS, Han IH, Lee IS, et al. Imaging findings of solitary spinal bony lesions and the differential diagnosis of benign and malignant lesions. J Korean Neurosurg Soc 2012;52:126-32. [Crossref] [PubMed]


