Assessing the effects of lumbar posterior stabilization and fusion to vertebral bone density in stabilized and adjacent segments by using Hounsfield unit
Introduction
Posterior lumbar stabilization with pedicle screw and fusion with bone graft is commonly used in the treatment of lumbar spinal spondylosis and stenosis (1). Evaluation of vertebral bone density before and after these surgeries is important to determine the presence of osteoporosis, so the risk of vertebral fracture and screw loosening can be predicted (2,3).
The term device-related osteoporosis is defined in the literature. Mineral bone density was assessed in canine models with histomorphometry. Lower bone density was found in fused spines versus un-fused spines. Rigid fixation resulted osteoporosis and increased spinal fusion rates (4).
Dual X-ray absorptiometry (DXA) is currently considered to be the gold standard for bone mineral density measurement. Use of DXA causes added costs and radiation. DXA is also not suitable for use in the patients with screw fixation (5).
Use of computed tomography (CT) to evaluate bone mineral density was suggested in some recent studies. The reliability and accuracy of Hounsfield units (HU) to determine osteoporosis were shown in the literature with many reports (6-8). HU may provide information regarding bone quantity that is readily available on CT scans without added costs and radiation.
Sacral screw failures are common problem in the lumbosacral fixation. There are many reports in the literature which intended to show the causes (9,10). In this presented study, we contributed to the literature by comparing lumbar vertebral body bone density with sacral vertebral body bone density.
Degeneration which develops at mobile segments above or below a fused spinal segment is known as adjacent segment disease (ASD) (11). Osteoporosis adjacent to a fusion is one of the forms of ASD. Although the exact mechanism remains uncertain, altered biomechanical stresses appear to play a key role in the development of ASD (12-15). Decrease of bone density of a vertebra in the stabilized segment is well-known entity but there is no study in the literature which showed the bone density of a vertebra in the adjacent segment.
In this retrospective study, we aimed to determine the bone density changes of the stabilized and adjacent segment vertebral bodies by comparing HU values before and after lumbar posterior stabilization. We tried to conclude that the decrease in the bone density of the adjacent segment vertebral bodies may be one of the major predisposing factors for adjacent segment fractures. We also discussed about sacral screw failures by comparing the HU values of sacral vertebral bodies with lumbar vertebral bodies.
Methods
We retrospectively studied 16 patients that underwent similar surgical procedures of L2-3-4-5 transpedicular screw fixation, fusion and L3-4 total laminectomy with similar diagnosis of lumbar spondylosis and stenosis between 2008 and 2014. There was no need for any approval for this retrospective study. The patients with postoperative spinal infections were excluded from this study. Mean age of the patients was 64 (range, 56–78) years. Nine of the all patients were male.
The patients who had preoperative and postoperative CT images in determined intervals were evaluated in this study. The time interval of preoperative CT and operation dates ranged from 1 to 7 days. The time interval of postoperative CT and operation dates ranged from 9 to 13 months.
A helical eight-channel CT scanner (LS; General Electric) was utilized for all measurements. CT parameters included a slice thickness of 1.25 mm with a 0.625-mm interval, a tube voltage of 120 kVp, a tube current of 300 mA (Smart mA/Auto mA range, 150–750), and a bone reconstruction algorithm (window width/window level, −3000/300). Two dimensional reconstructions were obtained in the coronal and sagittal planes.
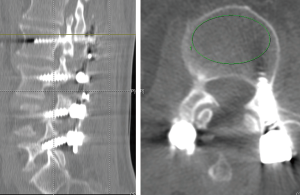
GE Universal Viewer was used to calculate an average HU value by placing an elliptical region of interest that was confined to the medullar space of the vertebral body to reduce the potential for beam hardening and volume averaging from the adjacent cortical bone and screw. Regions of interest were measured on the axial images. Locations of inferior to the superior end plate and superior to the screws were used for the patients with lumbar spine instrumentation (Figures 1,2). A mean HU value for each lumbar vertebra was recorded pre and postoperatively.

Results were evaluated by statistical analysis. Data are expressed as mean ± standard deviation (SD). Paired-Samples t-test was used to compare the two periods for each groups. Analysis of Variance was used to compare the regions among groups. For post-hoc comparisons between the pair-wise groups, the Tukey HSD test was used. Statistical analysis was performed by using commercial software (IBM SPSS Statistics 19, SPSS Inc., an IBM Co., Somers, NY, USA).
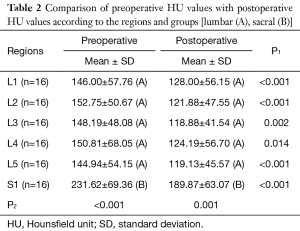
Values are expressed as mean ± SD. For region factor different uppercase letters (A, B) in the same column. ANOVA indicated a statistical significant difference. P1 showed comparisons between periods (Paired-Samples t-test). P2 showed comparisons among groups.
Results
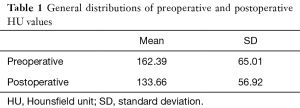
We compared preoperative bone density value of the vertebral body with postoperative bone density value of the same vertebral body. The HU values obtained from CT were stratified by preoperative and postoperative values. The mean and SD of preoperative HU value was found to be as 162.39±65.01. The mean and SD of postoperative HU value was found to be as 133.66±56.92 (Tables 1,2).
Full table
Full table
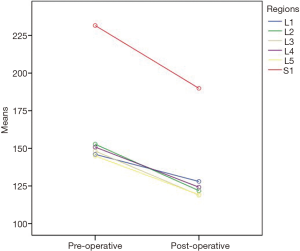
We found significant differences between preoperative and postoperative vertebral bone density values in the stabilized segments (L2, 3, 4, 5). There were significant HU decreases in the L2 (P<0.001), L3 (P=0.002), L4 (P=0.014) and L5 (P<0.001) vertebra after the operations (Figure 3).
Moreover, we found significant differences between preoperative and postoperative vertebral bone density values in the adjacent segments (L1, S1). There were significant HU decreases in the L1 (P<0.001) and S1 (P<0.001) vertebra after the operations (Figure 3).
We also compared S1 HU values with L1-5 HU values pre and postoperatively. We found significant differences between S1 HU values with L1-5 HU values in the preoperative and postoperative groups. S1 HU values were found to be significantly higher than L1-5 HU values in the preoperative group (P<0.001) and postoperative group (P=0.001) (Figure 3).
Discussion
There are some recent reports in the literature demonstrated that regional bone mineral density could be approximated from HU measured on CT. The HU value was found to correlate with T-scores, which are used in the WHO guidelines to diagnose osteoporosis (6-8). There is also very well-known entity that, DXA has limited value for the patients with lumbar instrumentation. Metallic rods or spinal fusion devices in the lumbar spine would preclude scanning at this site (16). Therefore, we used HU to analysis vertebral bone density.
HU was used to assess osteoporosis, bone graft fusion and spinal fusion success in some reports in the literature (17-19). We used HU to assess the effects of lumbar posterior stabilization to the vertebral bone density in the stabilized and adjacent segments. We selected the patients who had similar surgical procedure with similar diagnosis in order to assess statistically.
Device related osteoporosis was shown by histomorphometric study. Operated and fused spines were compared with non-operated and non-fused spines. Lower bone densities were found in fused spines versus un-fused spines (4). In this presented study; we found significant HU value decreases in all fused spines after the operations when we compared with same spines before the operations. Posterior lumbar stabilization caused decreases of vertebral bone density in all stabilized segments (L2, 3, 4, 5). Some studies emphasized that this condition does not cause increased risk of fracture because the increase in cross-sectional area and fusion mass of the vertebra (20,21). We also did not experience vertebral fracture in the stabilized segments in this presented study.
Providing adequate lumbosacral junction fixation is an important and challenging problem. Sacral screw failures are more common entity than lumbar screw failures. Bone quality, purchase of cortical bone, and screw length with bicortical purchase in the S1 pedicle were shown as most important criteria for adequate sacral fixation (9,10,22). Additionally the centrum of the vertebral body was found to be stronger than sacral ala in multiple load-to-failure tests (22). In this study, we found significantly higher HU values in the sacral vertebral bodies than lumbar vertebral bodies preoperatively and postoperatively. Sacral vertebral bodies were found to be stronger than lumbar vertebral bodies with higher bone densities. So the most important reasons for sacral screw failures are probably short anterior-posterior diameter in the sacral vertebral body, absence of cortical structure in the sacral pedicle and inadequate sacral fixation technique.
ASD is a very serious problem for the patients who underwent lumbar posterior stabilization. Abnormal processes that develop next to spinal fusions are referred to as ASD. Many processes are accepted as ASD such as listhesis, instability, hypertrophic facet, adjacent vertebral compression fracture, spinal canal stenosis and disc degeneration. ASD was found to be the most common reason for revision surgery. Some theories have been proposed to explain these processes. Most accepted opinion is that: fused lumbar segments increase stress and motion at the adjacent unfused segments accelerating degeneration of these segments. Other processes causing to ASD include increased age, osteopenia, preoperative comorbidities, thoracoplasty, male sex, rigid implant systems, preoperative hyperkyphotic thoracic alignment, post-operative sagittal imbalance, sagittal imbalance associated with hip and knee degeneration, and acute corrections of sagittal malalignment (11-15). In this presented study we found decreases of vertebral bone density in adjacent segment vertebral bodies postoperatively when we compared with same vertebral bodies preoperatively. Posterior lumbar stabilization caused HU decreases of vertebral bone density in the adjacent segments as in the stabilized segments. This condition may be due to prolonged periods of inactivity. So unloading of the skeleton promotes reduced bone mass. Limited motion and pain may cause reducing activity.
There is no study in the literature which shows vertebral bone density in adjacent segments for the patients with posterior lumbar stabilization. According to our opinion; decrease of vertebral bone density in the adjacent segments may be one of the main causes of adjacent segment fractures. This condition also may be related with degenerative processes of the vertebra in the adjacent segments. High rates of adjacent vertebral fractures, degenerations and subluxations have been described with lumbar fusions in the literature (23,24). The strengthening vertebral bone of adjacent lumbar spine with vertebroplasty and kyphoplasty was shown to be related with reduce the incidence of adjacent vertebral fracture. Additionally, lower bone density assessed with HU measurements was found to be associated with adjacent segment fracture after spinal fusion surgery (25). Therefore, in the view of the results of our study and the studies in the literature, strengthening vertebral bone of adjacent lumbar spine with surgical or medical therapy before spinal fusion surgeries may reduce the occurrence of adjacent segment fractures.
Limitations
In this study, we evaluated matched patients retrospectively. Our study comprised limited number of patients with limited follow up. Additionally, although we reported the issue which is not previously reported in the literature, we can not present any data to support causations. A long-term follow-up of a cohort of patients with posterior lumbar stabilization and normal controls will highly be recommended to provide further evidence on causations.
Conclusions
Posterior stabilization and fusion caused decreases in the bone density of the stabilized and the adjacent segment lumbar and sacral vertebral bodies. Posterior stabilization and fusion may protect stabilized vertebral segment. Therefore, the vertebra in the adjacent segments seems to be at greater risk of complications such as ASD.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Weinstein JN, Boden SD, An H. Emerging technology in spine: should we rethink the past or move forward in spite of the past? Spine (Phila Pa 1976) 2003;28:S1. [Crossref] [PubMed]
- Link TM, Koppers BB, Licht T, et al. In vitro and in vivo spiral CT to determine bone mineral density: initial experience in patients at risk for osteoporosis. Radiology 2004;231:805-11. [Crossref] [PubMed]
- Miyabara Y, Holmes D 3rd, Camp J, et al. Comparison of calibrated and uncalibrated bone mineral density by CT to DEXA in menopausal women. Climacteric 2012;15:374-81. [Crossref] [PubMed]
- McAfee PC, Farey ID, Sutterlin CE, et al. 1989 Volvo Award in basic science. Device-related osteoporosis with spinal instrumentation. Spine (Phila Pa 1976) 1989;14:919-26. [Crossref] [PubMed]
- Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 1996;312:1254-9. [Crossref] [PubMed]
- Lee S, Chung CK, Oh SH, et al. Correlation between Bone Mineral Density Measured by Dual-Energy X-Ray Absorptiometry and Hounsfield Units Measured by Diagnostic CT in Lumbar Spine. J Korean Neurosurg Soc 2013;54:384-9. [Crossref] [PubMed]
- Schreiber JJ, Anderson PA, Rosas HG, et al. Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Joint Surg Am 2011;93:1057-63. [Crossref] [PubMed]
- Schreiber JJ, Anderson PA, Hsu WK. Use of computed tomography for assessing bone mineral density. Neurosurg Focus 2014;37:E4. [Crossref] [PubMed]
- McCall T, Fassett D, Dailey A. Sacral Screw Fixation. Spine Trauma: Surgical Techniques 2010;335-40.
- Smith SA, Abitbol JJ, Carlson GD, et al. The effects of depth of penetration, screw orientation, and bone density on sacral screw fixation. Spine (Phila Pa 1976) 1993;18:1006-10. [Crossref] [PubMed]
- Anderson CE. Spondyloschisis following spine fusion. J Bone Joint Surg Am 1956;38-A:1142-6. [Crossref] [PubMed]
- Kumar MN, Jacquot F, Hall H. Long-term follow-up of functional outcomes and radiographic changes at adjacent levels following lumbar spine fusion for degenerative disc disease. Eur Spine J 2001;10:309-13. [Crossref] [PubMed]
- Lee CK. Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine (Phila Pa 1976) 1988;13:375-7. [Crossref] [PubMed]
- Park P, Garton HJ, Gala VC, et al. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976) 2004;29:1938-44. [Crossref] [PubMed]
- Wimmer C, Gluch H, Krismer M, et al. AP-translation in the proximal disc adjacent to lumbar spine fusion. A retrospective comparison of mono- and polysegmental fusion in 120 patients. Acta Orthop Scand 1997;68:269-72. [Crossref] [PubMed]
- Baim S, Binkley N, Bilezikian JP, et al. Official Positions of the International Society for Clinical Densitometry and executive summary of the 2007 ISCD Position Development Conference. J Clin Densitom 2008;11:75-91. [Crossref] [PubMed]
- Schwaiger BJ, Gersing AS, Baum T, et al. Bone mineral density values derived from routine lumbar spine multidetector row CT predict osteoporotic vertebral fractures and screw loosening. AJNR Am J Neuroradiol 2014;35:1628-33. [Crossref] [PubMed]
- Spruit M, Meijers H, Obradov M, et al. CT density measurement of bone graft within an intervertebral lumbar cage: increase of hounsfield units as an indicator for increasing bone mineral content. J Spinal Disord Tech 2004;17:232-5. [Crossref] [PubMed]
- Wittenberg RH, Shea M, Swartz DE, et al. Importance of bone mineral density in instrumented spine fusions. Spine (Phila Pa 1976) 1991;16:647-52. [Crossref] [PubMed]
- Farey ID, McAfee PC, Gurr KR, et al. Quantitative histologic study of the influence of spinal instrumentation on lumbar fusions: a canine model. J Orthop Res 1989;7:709-22. [Crossref] [PubMed]
- McAfee PC, Farey ID, Sutterlin CE, et al. The effect of spinal implant rigidity on vertebral bone density. A canine model. Spine (Phila Pa 1976) 1991;16:S190-7. [Crossref] [PubMed]
- Baldwin NG, Benzel EC. Sacral fixation using iliac instrumentation and a variable-angle screw device. Technical note. J Neurosurg 1994;81:313-6. [Crossref] [PubMed]
- Ahn Y, Lee SH. Vertebroplasty for adjacent vertebral fracture following lumbar interbody fusion. Br J Neurosurg 2011;25:104-8. [Crossref] [PubMed]
- Toyone T, Ozawa T, Kamikawa K, et al. Subsequent vertebral fractures following spinal fusion surgery for degenerative lumbar disease: a mean ten-year follow-up. Spine (Phila Pa 1976) 2010;35:1915-8. [Crossref] [PubMed]
- Yen CH, Teng MM, Yuan WH, et al. Preventive vertebroplasty for adjacent vertebral bodies: a good solution to reduce adjacent vertebral fracture after percutaneous vertebroplasty. AJNR Am J Neuroradiol 2012;33:826-32. [Crossref] [PubMed]


