Radiological factors affecting post-operative global coronal balance in Lenke 5 C scoliosis
Introduction
Lenke 5 C scoliosis is frequently associated with clinical and radiological evidence of global coronal imbalance (1,2). The appropriate selection of levels for proximal and distal extent of instrumentation has a direct impact on the coronal balance, curve correction and radiological outcome of a well-balanced spine following surgery (3-6). Lenke 5 C curves have been treated by anterior or posterior approaches with good results being quoted by both techniques (6-10). Although posterior selective instrumented deformity correction is being favored more recently (7-9,11), there is no consensus on the selection of proximal and distal levels for fusion based on objectively assessed criteria (2,12).
Selective fusion of the structural curve with an expectation of spontaneous correction of the non-structural compensatory curve is the basis of the selective posterior deformity correction (13-16). However, in Lenke 5 C, immediate post-operative and late decompensation of coronal balance have been noted with selective posterior deformity correction (1,2,17). Spontaneous correction of the compensatory curve and well a balanced spine as achieved with selective thoracic fusion in Lenke 1 and 2 curves is based on an objective assessment of the curve (3,5,14,18,19). Similar objective criteria, to assess feasibility of selective fusion in Lenke 5 C curves, to ensure a well balance coronal correction have not been defined. As a result, comparable and reliable correction results as seen with selective thoracic fusion have not been replicated with posterior correction of Lenke 5 C curves (20).
We aimed to evaluate the short term and long term radiological outcome of patients with Lenke type 5C scoliosis treated with posterior instrumented correction. We assessed this on the following points (I) radiological factors that were associated with global coronal imbalance in the early post-operative period; (II) factors concerned with late decompensation of coronal balance; and (III) factors associated with late favourable spontaneous correction of coronal imbalance on long term follow up.
Methods
Between January 2010 and January 2013, 23 consecutive Lenke 5 C adolescent idiopathic scoliosis (AIS) patients who underwent selective posterior pedicle screw instrumentation were included in this study for retrospective analysis. Institutional review board approval was obtained for the study. Inclusion criteria for the analysis were AIS with major thoracolumbar/lumbar curve classified as Lenke type 5 C that underwent a one-stage selective posterior surgery.
Surgical approach
All patients were operated by two senior surgeons. Pedicle screw and rod manipulating techniques were performed according to Scoliosis research society recommendations and included rod rotation, distraction on concave side, compression on convex side and in situ rod bending. In some rigid curves, multiple level posterior releases and Ponte osteotomies were performed. Fusion levels were based on surgeon’s preference.
Radiographic measurements
Assessment of pre-operative, early post-operative and late follow up radiographs was done using VEPRO software. It included upright pre-operative posteroanterior (PA), lateral standing radiographs and supine right and left bending films. Early post-operative radiographs were taken at a period between 7–10 days following surgery and late follow-up radiographs at 2-year follow-up. Cobb angles, lumbar lordosis, global coronal balance, upper instrumented vertebra (UIV) tilt and translation, lower instrumented vertebra (LIV) tilt and translation were documented (Figure 1).
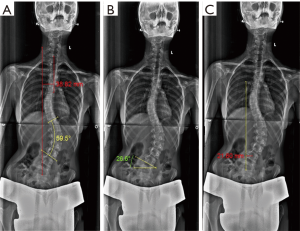
Global coronal balance: Measured in millimetres as the perpendicular distance between C7 plumb line and the central sacral vertical line (C7-CSVL). A deviation over 20 mm was defined as coronal imbalance.
UIV and LIV translation: Defined as distance in millimetres from the geometric centre of the UIV and LIV to the CSVL.
UIV and LIV tilt: Defined as the inclination of superior end plate to the horizontal for the UIV and of the inferior endplate to the horizontal for the LIV.
LIV disc angle: Defined as the angle subtended between the inferior endplate of LIV relative to the superior endplate of the next caudal vertebra. The change in disc angle was calculated by subtracting the right side bending LIV disc angle from the left side-bending LIV disc angle.
Statistical analyses
The data was analysed using SPSS 16.0 statistical software (SPSS Inc., Chicago, IL). Pearson correlation and linear regression were used to analyse the correlation of each parameter to global coronal balance and regional coronal balance (LIV translation and UIV translation). All the data were presented as mean ± standard deviation. Paired student’s t test was utilized to assess differences between radiographic parameters at three time points (pre-operative, early post-operative and late follow-up). Correlation values of “r” were defined as follows: high correlation (0.80–1.00), marked correlation (0.60–0.79), moderate correlation (0.40–0.59) and <0.40 noted as low or no correlation. Statistical significance was defined as P<0.05.
Results
Patient demographics
A total of 30 patients with Lenke 5 C curves underwent surgery during the study period. Five patients had an associated significant shoulder asymmetry or prominent rib hump thus; the fusion was extended to T4. Two patients were lost during follow up leaving 23 cases for the final analysis. There were 21 females and 2 males with a mean age of 15.2±3 years. The mean Risser grade was 3.0±1.68 and mean patient follow up duration was for 36 months.
Selection of fusion levels
Twenty-two patients had left sided curve and one patient had right sided curve. Twelve patients had the upper end vertebra (UEV) at T10 and in remaining 11 patients the UEV was T11. In 11 patients, the lower end vertebra (LEV) was L3 and 12 patients had end vertebra at L4. UIV was T10 in 13 patients and T11 in 4 patients. In 19 patients the LIV was L4. The UIV was equal to UEV (UIV = UEV) in 11 patients, 1 above the UEV (UIV = UEV+1) in eight patients, 2 above the UEV (UIV = UEV+2) in three patients, and 3 above the UEV (UIV = UEV+3) in one patient. The LIV was equal to LEV (LIV = LEV) in 12 patients, one level below the LEV (LIV = LEV+1) in ten patients, 2 below the LEV (LIV = LEV+2) in one patient.
Curve characteristics
The pre-operative and post-operative characteristics of the curves are presented in Table 1. The mean pre-operative Cobb angle of thoracolumbar/lumbar (TL/L) curve was 55.01˚±13.26˚, with mean side bending angle of 29.73˚±17.83˚, reflecting mean curve flexibility of 47.86%±21.51%. The average immediate post-operative Cobb angle was 14.68˚±8.84˚. Late post-operative Cobb angle was 15.19˚±8.91˚, reflecting the mean correction rate of 72.39% with a significant deformity correction (P<0.001). The mean pre-operative LIV disc angle was 5.31˚±2.87˚. The mean post-operative LIV disc angle at last follow up was of 2.2˚±2.75˚. The average LIV disc angle change was 3.7˚±3.32˚.
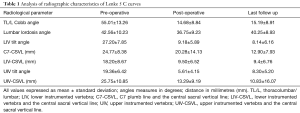
Full table
The mean pre-operative lordosis was 42.56˚±10.23˚ and the mean post-operative lordosis at last follow up was 40.25˚±8.93˚. The mean pre-operative LIV tilt was 27.2˚±7.85˚ and mean post-operative LIV tilt at final follow up was 8.14˚±6.16˚ and the difference was statistically significant (P<0.001). The mean pre-operative UIV tilt was 19.36˚±6.42˚, and early post-operative tilt was 5.61˚±4.15˚. At the last follow up UIV tilt increased to the mean of 8.3˚±5.2˚.
Coronal balance
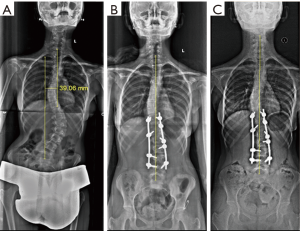
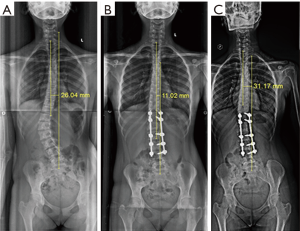
The average pre-operative C7-CSVL (global coronal balance) was 24.77±8.38 which improved to 12.9±7.93 mm and the difference was statistically significant (P<0.001). The average pre-operative LIV-CSVL (LIV translation) was 18.2±8.67 mm. In early post-operative period, there was a significant (P<0.001) decrease in mean LIV-CSVL distance (9.5±6.52 mm) and the difference was maintained on late follow up. Figure 2 shows a case which showed good radiological outcome with good coronal balance on early and late follow up.
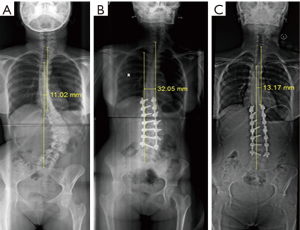
The mean pre-operative and late post-operative UIV-CSVL (UIV translation) was 25.75±10.85 and 10.83±16.07 mm respectively. In our cohort 34.8% (n=8) patients had coronal imbalance in immediate post-operative period. Out of 8 patients 75% (6/8) patients were coronally balanced at the last follow up (Figure 3). Four patients had post-operative coronal imbalance on late follow up. This includes two patients with early post-operative coronal imbalance which persisted on late follow up. We also had two cases that had a satisfactory early post-operative radiograph but developed late post-operative coronal imbalance (Figure 4). All the four patients which had late coronal imbalance had pre-operative coronal imbalance with a pre-operative LIV tilt >25° which was statistically significant. These four patients also had a post-operative LIV tilt >8°.
Radiographic parameters which correlated with coronal imbalance were pre-operative LIV tilt (r=0.64, P=0.001), pre-operative LIV-CSVL distance (r=0.696, P<0.001), pre-operative UIV translation (r=0.44, P=0.030), early post-operative LIV tilt (r=0.804, P<0.001), and early post-operative UIV tilt (r=0.62, P=0.001). No instrument related complications were noted till last follow up.
Discussion
Studies have shown comparable results with anterior instrumentation or posterior pedicle screw instrumentation in the surgical correction of Lenke 5 C idiopathic scoliosis (6-11). Any selective posterior fusion for either the thoracic curve or the thoracolumbar/lumbar curve is performed with the expectation of spontaneous correction of the minor curve (5,20). Elaborate criteria have been enlisted for appropriate selection of Lenke 1, 2 and 3 with C modifiers for possible selective fusion of the thoracic curve (3,5,14,18,19) When these criteria of selective thoracic fusion are adhered to good spontaneous correction of the lumbar C modifier curve has been observed (5,14,16). However, such a similar selection criterion for thoracolumbar/lumbar scoliosis has not been clearly defined. The spontaneous minor curve corrections as seen with Lenke 1 C have not been replicated in Lenke 5 C (20).
A good coronally well balanced spine is the final aim of any scoliosis deformity correction surgery. Frequently Lenke 5 C curves following selective posterior or anterior deformity correction may be left with residual coronal imbalance (1,2,17). Very few studies have analysed selective posterior pedicle screw based Lenke 5 C correction procedures, to identify radiological factors that are associated with early or late post-operative coronal imbalance. An identification of such factors associated with coronal imbalance may be useful to develop objective criteria for appropriate selection of cases of Lenke 5 C which can undergo selective fusion of the lumbar curve.
We looked at radiographs at 3 points of time- pre-operative, early post-operative and late post-operative (>2 years) to identify radiological parameters which may be associated with coronal imbalance. We had eight cases with early post-operative coronal imbalance however, 6 had spontaneous resolution on late follow up. Out of the eight cases with early post-operative coronal imbalance 5 had a LIV tilt of >25°. Considering radiological outcome on late follow up there were four cases with coronal imbalance. Two cases with coronal imbalance persisting from the early post-operative period and two cases developed coronal imbalance where early post-operative radiographs had satisfactory coronal alignment. In our study 16 patients had LIV tilt >25˚ and 5 (31%) of these were coronally imbalanced in early post-operative period.
In the coronally imbalanced patients, the mean post-operative LIV tilt was 11.7˚, and in coronally balanced patients the post-operative LIV tilt was 7.6˚. Li et al. noted that failure of LIV tilt to reduce below 8˚ correlated with high risk of coronal imbalance (17). This finding is in agreement with our results that cases with high post-operative LIV tilt are at high risk of coronal imbalance. Li et al. also noted that pre-operative LIV tilt correlated with post-operative global and regional coronal balance, and pre-operative LIV tilt ≥25˚ correlated with high risk of developing global coronal imbalance (17).
Liu et al. recognized the significance of UIV tilt in final outcome of coronal balance (1). According to them, only the final UIV tilt inversely correlated with the ultimate coronal balance. They concluded that UIV tilt compensates for the coronal imbalance in the immediate post-operative period and in most of the cases the coronal balance improves in late follow up period by increasing the UIV tilt. In our study, eight patients were coronally imbalanced in the early post-operative period and six patients improved and were coronally balanced at the last follow up. Amongst these six patients, four patients had an increase in UIV tilt at the last follow up. Therefore, UIV tilt could be considered a factor affecting coronal balance.
The choice of LIV has been the subject of debate when discussing anterior vs. posterior correction in Lenke 5 C. In our study in 52.17% (n=12) patients, LIV was at the level of LEV (LIV = LEV) and in 43.48% (n=10) patients the LIV was LEV+1. L4 was the lowest instrumented vertebra in 82.6% cases. The LIV was 2 below the LEV (LIV = LEV+2) in one patient.
In the study by Geck et al. LIV = LEV (L3) in 87% cases (n=27) and LEV+1 (L4) in 12% (n=4) cases. In both the groups coronal balance was maintained post-operatively, but the patients whose fusion went up to L4 (LEV+1) had better results with LIV translation thereby implying lower regional imbalance (8).
Post-operative coronal imbalance correlated with pre-operative LIV tilt (r=0.64, P=0.001), pre-operative LIV-CSVL distance (r=0.696, P<0.001), early post-operative LIV tilt (r=0.804, P<0.001), and early post-operative UIV tilt (r=0.62, P=0.001). Li et al. analysed 27 cases of Lenke 5 C treated with posterior deformity correction and noted three factors which affected radiological outcomes which included, pre-operative coronal imbalance, pre-operative LIV tilt and post-operative LIV tilt (17). Wang et al. reported on 30 cases of Lenke 5 C treated with selective fusion and noted pre-operative LIV-CSVL more than 28 mm and LIV tilt ≥25° as factors which were associated with coronal imbalance (2). More recently Liu and colleagues showed in an analysis of 40 cases that parameters significantly associated with coronal imbalance were pre-operative coronal imbalance and pre-operative LIV and they showed an inverse relation with UIV tilt and coronal imbalance (1). In summary the findings of the current study are in agreement with previous literature on possible factors relating to coronal imbalance in Lenke 5 C. The factors which are most significantly related are pre-operative LIV tilt, post-operative LIV tit and pre-operative coronal imbalance. Increasing UIV tilt offers a possible explanation of late improvement in coronal balance in cases which showed less than satisfactory results in the early post-operative period. The limitations of this study include retrospective study design and small sample size for assessment.
Conclusions
In Lenke 5 C scoliosis, posterior pedicle screw instrumentation gives good coronal and sagittal correction which is maintained in late follow up period. Pre-operative LIV tilt significantly correlates with post-operative global imbalance and a higher pre-operative LIV tilt ≥25° have a higher risk of developing coronal imbalance. Increasing UIV tilt may be a factor associated with improving coronal balance in late follow up period. L4 as the LIV gave good radiological outcome in our patients and (LEV+1) may be considered satisfactory. However, cases with LIV tilt >25° are prone to get late post-operative coronal imbalance and this should be factored when choosing the LIV.
Acknowledgements
The project was funded by Ganga Orthopaedic Research & Education Foundation, Coimbatore.
Footnote
Conflicts of Interest: The authors have no conflict of interest to declare.
Ethical Statement: Institutional review board approval was obtained for the study. Informed written consent has been obtained from the participants.
References
- Liu Z, Guo J, Zhu Z, et al. Role of the upper and lowest instrumented vertebrae in predicting the postoperative coronal balance in Lenke 5C patients after selective posterior fusion. Eur Spine J 2013;22:2392-8. [Crossref] [PubMed]
- Wang Y, Bünger CE, Zhang Y, et al. Lowest instrumented vertebra selection for Lenke 5C scoliosis: a minimum 2-year radiographical follow-up. Spine (Phila Pa 1976) 2013;38:E894-900. [Crossref] [PubMed]
- Ishikawa M, Cao K, Pang L, et al. Postoperative behavior of thoracolumbar/lumbar curve and coronal balance after posterior thoracic fusion for Lenke 1C and 2C adolescent idiopathic scoliosis. J Orthop Sci 2015;20:31-7. [Crossref] [PubMed]
- Suk SI, Lee SM, Chung ER, et al. Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: more than 5-year follow-up. Spine (Phila Pa 1976) 2005;30:1602-9. [Crossref] [PubMed]
- Fischer CR, Kim Y. Selective fusion for adolescent idiopathic scoliosis: a review of current operative strategy. Eur Spine J 2011;20:1048-57. [Crossref] [PubMed]
- Wang Y, Fei Q, Qiu G, et al. Anterior spinal fusion versus posterior spinal fusion for moderate lumbar/thoracolumbar adolescent idiopathic scoliosis: a prospective study. Spine (Phila Pa 1976) 2008;33:2166-72. [Crossref] [PubMed]
- Shufflebarger HL, Geck MJ, Clark CE. The posterior approach for lumbar and thoracolumbar adolescent idiopathic scoliosis: posterior shortening and pedicle screws. Spine (Phila Pa 1976) 2004;29:269-76. [Crossref] [PubMed]
- Geck MJ, Rinella A, Hawthorne D, et al. Comparison of surgical treatment in Lenke 5C adolescent idiopathic scoliosis: anterior dual rod versus posterior pedicle fixation surgery: a comparison of two practices. Spine (Phila Pa 1976) 2009;34:1942-51. [Crossref] [PubMed]
- Hee HT, Yu ZR, Wong HK. Comparison of segmental pedicle screw instrumentation versus anterior instrumentation in adolescent idiopathic thoracolumbar and lumbar scoliosis. Spine (Phila Pa 1976) 2007;32:1533-42. [Crossref] [PubMed]
- Liljenqvist U, Halm H, Bullmann V. Spontaneous lumbar curve correction in selective anterior instrumentation and fusion of idiopathic thoracic scoliosis of Lenke type C. ur Spine J 2013;22:S138-48. [Crossref] [PubMed]
- Bennett JT, Hoashi JS, Ames RJ, et al. The posterior pedicle screw construct: 5-year results for thoracolumbar and lumbar curves. Journal of Neurosurgery Spine 2013;19:658-63. [Crossref] [PubMed]
- Sanders AE, Baumann R, Brown H, et al. Selective anterior fusion of thoracolumbar/lumbar curves in adolescents: when can the associated thoracic curve be left unfused? Spine (Phila Pa 1976) 2003;28:706-13. [Crossref] [PubMed]
- Jansen RC, van Rhijn LW, Duinkerke E, et al. Predictability of the spontaneous lumbar curve correction after selective thoracic fusion in idiopathic scoliosis. Eur Spine J 2007;16:1335-42. [Crossref] [PubMed]
- Lenke LG, Edwards CC 2nd, Bridwell KH. The Lenke classification of adolescent idiopathic scoliosis: how it organizes curve patterns as a template to perform selective fusions of the spine. Spine (Phila Pa 1976) 2003;28:S199-207. [Crossref] [PubMed]
- Dobbs MB, Lenke LG, Walton T, et al. Can we predict the ultimate lumbar curve in adolescent idiopathic scoliosis patients undergoing a selective fusion with undercorrection of the thoracic curve? Spine (Phila Pa 1976) 2004;29:277-85. [Crossref] [PubMed]
- Schulte TL, Liljenqvist U, Hierholzer E, et al. Spontaneous correction and derotation of secondary curves after selective anterior fusion of idiopathic scoliosis. Spine (Phila Pa 1976) 2006;31:315-21. [Crossref] [PubMed]
- Li J, Hwang SW, Shi Z, et al. Analysis of radiographic parameters relevant to the lowest instrumented vertebrae and postoperative coronal balance in Lenke 5C patients. Spine (Phila Pa 1976) 2011;36:1673-8. [Crossref] [PubMed]
- Chang KW, Leng X, Zhao W, et al. Broader curve criteria for selective thoracic fusion. Spine (Phila Pa 1976) 2011;36:1658-64. [Crossref] [PubMed]
- Chang KW, Chen YY, Wu CM, et al. Could structural and noncompensatory Lenke 3 and 4C lumbar curves be nonstructural and compensatory? Lenke 1, 2, 3, and 4 Curve Types were similar and could be considered collectively as a single indication for selective thoracic fusion. Spine (Phila Pa 1976) 2014;39:1850-9. [Crossref] [PubMed]
- Ritzman TF, Upasani VV, Bastrom TP, et al. Comparison of compensatory curve spontaneous derotation after selective thoracic or lumbar fusions in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2008;33:2643-7. [Crossref] [PubMed]


