Does the law of diminishing returns apply to the lengthening of the MCGR rod in early onset scoliosis with reference to growth velocity?
Introduction
The surgical management of early onset scoliosis (EOS) is based around controlling the scoliotic curve whilst allowing continued growth of the thorax for maximum lung development (1,2). The MAGnetic Expansion Control Growth Rod (MCGR, NuVasive, San Diego, CA, USA) was licensed by the National Institute of Clinical Excellence (NICE) in the UK in 2014 (3). MCGR is an evolution of traditional growth rods (TGR) for the management of EOS and is reported to be safe and reliable (4-6). The MCGR functions on the same principal as the TGR, allowing control of the scoliotic curve without fusion of the spine so that spinal growth and thus thoracic and lung growth can continue (7). MCGR are different from TGR in that the ‘lengthening’ procedures are performed remotely in the outpatient setting rather than requiring repeat mechanical lengthening under general anaesthesia with a surgical approach and exposure of the implants.
It has been reported previously (8) that there is a ‘law of diminishing returns’ with TGR. This is where, on repeated lengthening episodes, the amount of length that is achieved decreases, such that after seven lengthening procedures, little length is gained.
It is unclear whether the ‘law of diminishing returns’ applies when MCGR are used in the setting of EOS. This paper reports on the experience of a single centre with a consecutive series of MCGR implanted to manage EOS and specifically examines whether the law of diminishing returns applies in a similar way to TGR. The paper then goes on to compare longitudinal growth of MCGR over serial lengthening with published growth data in the non-scoliotic spine.
Methods
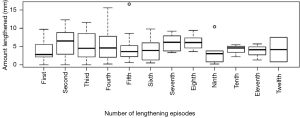
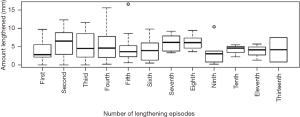
A retrospective review of a consecutive series of MCGRs implanted for the management of EOS was conducted. This group with EOS was a heterogenous group of diagnoses as would be seen in every day clinical practice. All of these rods were lengthened in the out-patient setting, in an awake child without the use of sedation. The MCGR was lengthened to as much as the child could tolerate comfortably or when the mechanism clunked repeatedly. The review included radiographs and hospital records. The diagnosis was identified along with the amount of length achieved which was measured from radiographs. The radiographs were measured from the hospital digital PACS system (Picture Archiving and Communication System, GE Centricity, Chicago, IL, USA). The radiographic measurements were calibrated for accuracy of measurement against the known diameter of the rod. The measurement used in this study was of the change in the rod length, measured as the increasing gap seen within the actuator mechanism of the rod (Figure 1). The total length of the rod, in either coronal or sagittal plane, or total spine length was not measured. Any MCGR that had failed for any reason was excluded from the analysis at the point of failure. All data to that point was kept in the analysis.
The only rods included were those implanted as the primary surgical treatment and not revision MCGR. Any exchange procedures from TGR to MCGR were excluded. Any revision MCGR to further MCGR were included to the point of failure of the primary MCGR that requiring revision. The standard practice in our institution is to lengthen as much as is tolerated by the child every three months. Radiographs are not taken at every visit, rather at every 6 months matching our historical TGR practice.
The data was analysed using descriptive statistics. For data with a normal distribution, parametric statistics (mean and standard deviation) were used. For data where the distribution was not normal non-parametric statistics are used [median and interquartile range (IQR)].
The amount of length that occurred at each lengthening episode measured from the radiographs was analysed. Analysis was performed using the Kruskal-Wallis test as the data was not normally distributed. This analysis was performed for the whole cohort and, as a subgroup, those who had undergone more than eight lengthening episodes (equivalent of 2 years since the MCGR was implanted). Statistical significance was defined as P<0.05.
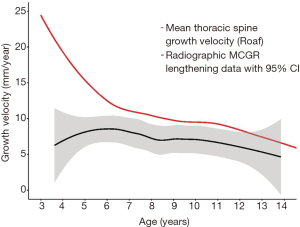
To examine the MCGR cohort as growth velocity, the growth from the MCGR cohort was then plotted against growth in a spine without scoliosis which was taken from previously published literature (9) and then transformed to growth velocity.
All analysis was performed using R (10).
This work was registered and approved with the local IRB (reference 16-040).
Results
There were 53 rods in 28 patients who all had a diagnosis of EOS, consisting of 10 males and 18 females. Double MCGR constructs were used in 25 patients, single constructs in 3 patients. One rod constructs were implanted if the child was particularly small and there was not enough soft tissue cover at the time of primary surgery to close the wound over two rods. The underlying diagnoses included idiopathic, neuromuscular, syndromic and congenital scoliosis and are shown in Table 1. The mean age of the cohort at the time of this review was 8 years 3 months (SD, 2 years 7 months; range, 3 years 6 months to 13 years 10 months). The mean follow-up period since primary rod implantation was 2 years 0 months (SD, 1 year 1 month; range, 8 months to 4 years 8 months). In the subgroup of those who were 2 or more years since implantation there were 6 patients with a mean follow up period of 2 years 9 months (SD, 8 months; range, 2 years 1 month to 4 years 2 months).

Full table
There were 11 rods removed from the analysis because of failure. The cause of this was infection in one rod, rod breakage outside the lengthening mechanism in 1 rod and a mechanical problem in the actuator demonstrated through failure to lengthen in 9 rods.
In the total cohort, the median number of MCGR lengthening episodes was 4 (IQR, 4; range, 1 to 12). The amount of growth per lengthening is shown in Figure 2 in a similar manner as that from Sankar et al. (8). Using the Kruskal-Wallis test there was no statistically significant difference between the number of lengthening episodes and the length achieved at that lengthening (P=0.427) for the overall cohort. In the subgroup the median number of lengthenings was 10 (IQR, 2; range, 9 to 12). Again, using the Kruskal-Wallis test there was no statistically significant difference between the number of lengthening episodes and the length achieved at that lengthening (P=0.438).
As shown in Figure 3, growth velocity from the cohort was plotted against the growth velocity of the thoracic spine taken from data previously published by Roaf (9) (red line). The velocity of the normal thoracic spine slows as the age of the child increases. There is a difference in velocity in absolute values (the growth velocity of the Roaf data is greater than that of the MCGR cohort by approximately 2–4 mm/year of growth from the age of 6 years). The gradient of the lines is similar and both decrease at a similar rate over the observed period.
Discussion
The aim of any growth friendly technology in the management of EOS is to control the scoliotic curve, minimising both the size and the rotation of the spine whilst allowing continued vertical growth. This philosophy aims to maximise the volume of the thorax allowing the best lung development for later life. Karol et al. (2) have shown that, in EOS, the thoracic spine height at maturity is associated with an increased risk of respiratory issues and associated morbidity in early adult life.
When using TGRs, the ‘law of diminishing returns’ can lead surgeons to be judicious about the age of the child when first implanting a TGR construct. This is because, on a 6-monthly lengthening schedule as suggested by Akbarnia et al. as giving the most reliable outcome with the least possible repeat procedures (11), seven lengthening episodes leads to the cessation of TGR treatment within three-and-a-half years of starting treatment (8).
The MCGR was designed to remove the need for repeated open surgical lengthening episodes and the MCGR is lengthened through the use of an external remote control. Early papers report that the MCGR allows longitudinal growth of the spine and is safe and reliable (4-6). A recent report of seven patients from Hong Kong has suggested that ‘frequent small distractions’ allowed continued gain in spinal length without a loss in the amount of length achieved over repeated lengthening episodes (12).
When the MCGR data presented here is regarded in a similar way to that of Sankar et al. (8), analysis shows that an increase in length of the spinal construct occurs at every lengthening episode and that this is maintained over serial lengthening episodes without a statistically significant reduction in length achieved. When looking only at the subgroup of this cohort who have had the MCGR implanted for at least two years, again lengthening occurs without a statistically significant decrease in length achieved over time. Thus, the conclusions here hold when those with a shorter follow up are eliminated. This is different to that seen in TGR where after seven lengthening episodes it was not possible to lengthen the TGR construct, and this agrees with the conclusions of Cheung et al. (12).
The reason for the “law of diminishing returns” in TGR is not clear. It is likely that the decreasing length achieved at each surgical lengthening is caused by a combination of stiffness over the instrumented levels from the spine and from the associated soft tissues around the spine. These soft tissues become progressively more scarred and stiff with each surgical lengthening which does not occur with an MCGR lengthening. The amount of desired length at each surgical lengthening episode is also greater in the TGR setting versus the MCGR setting, meaning that a greater force is applied to the spine and surrounding tissues. The MCGR lengthening frequency used here is twice that of the historic TGR cohort allowing smaller, more frequent distractions as described by Cheung et al. (12). We feel that these two differences between TGR and MCGR account for the difference between the length achieved over repeated lengthening in the different constructs. It is of note that Spurway et al. (13) has questioned the validity of the ‘law of diminishing returns’ as a concept suggesting it is related to the measurement of the length of the spine in the coronal plane which may be foreshortened because of kyphosis rather than what is the true length of the spine when measured in the sagittal plane. It is our practice to obtain radiographs in one plane only unless otherwise indicated due to concerns over the cumulative radiation dose to the children (14). We do not have the sagittal radiographs to comment further on this other than noting that our method of measurement of the change of the MCGR actuator rather than the T1–S1 height avoids this issue, although it is then only a surrogate measure for overall spinal height.
When the data is transformed in to growth velocity and the MCGR cohort is compared to published normative values for the growth velocity of the thoracic spine, the growth velocity of the MCGR is less than the norms. However, a velocity is maintained that decreases at a similar rate to that of the normative data.
The use of growth velocity, rather than the total number of lengthening episodes independent of the age of the child, is a better measure of the success of the system at maintaining spinal growth. The growth charts of the World Health Organisation (15) and the Centre for Disease Control (16) are based on age acknowledging that growth is age dependent. It is acknowledged that the growth velocity calculated from the data from Roaf (9) is the thoracic spine only and none of this series of MCGRs instrument wholly in the thoracic spine. Rather children were routinely instrumented from the upper thoracic spine (T3), across the thoracolumbar junction to mid lumbar spine (L3). The Roaf data is also not subdivided for sex. It is, however, growth data for a normal thoracic spine and is the best standard that could be found for comparative analysis. The MCGR cohort reflects the mix of underlying diagnoses that comprise EOS. It is not known what the expected growth should be in Marfans syndrome EOS versus a neurofibromatosis EOS versus an idiopathic EOS. Combining all of the data from this cohort will lose the individual variation seen in a particular condition. However, this heterogenous group does reflect modern practice and so analysis of the whole group as one is felt to be reasonable. Whilst surgical practice is to aim for the maximum possible length of the spinal construct, it may be appropriate to temper this with an expectation of what growth should be for the age of the child.
It is accepted that this paper examines each rod individually rather than as a pair. There has been no account taken of MCGR orientation (standard versus offset) or of implant type, the order that the rods were lengthened (convexity or concavity first) or the implant pattern connecting the MCGR to the spine. This methodology is however felt to be reasonable given the question posed which is only looking at the ability of the MCGR to continue lengthening after repeated lengthening episodes following implantation. The group is heterogeneous with regards diagnosis, age and sex. This is as seen in the paper by Sankar et al. (8) and reflects true clinical practice and is therefore applicable to other centres. It is also noted that the amount of length achieved per lengthening is not uniform between children or between different lengthening episodes in the same children. This again reflects real clinical practice in an awake child. Whilst the amount of length that can be seen in MCGR lengthenings can vary it must be borne in mind that the most accurate method of measurement of lengthening is against a standardised measure such as the known diameter of the rod by either radiography or ultrasound. Reliance solely on the external lengthening device may lead to both over or under estimate of the length gained.
In conclusion, the use of the MCGR in EOS does not follow the ‘law of diminishing returns’ and this represents an advantage to the use of MCGR over TGR. When examined against normative data for the growth velocity of the thoracic spine, MCGRs demonstrate the maintenance of growth velocity, although to a lesser degree than the normative values. It is felt that growth velocity is a more useful way of monitoring growth during the use of an MCGR construct for EOS than an absolute value for the number of lengthening episodes given that growth is age dependent.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This research study has IRB approval via the host institution (reference 16-040), and it conforms to the provisions of the Declaration of Helsinki (as revised in Edinburgh 2000).
References
- Thompson GH, Akbarnia BA, Campbell RM Jr. Growing rod techniques in Early-Onset Scoliosis. J Pediatr Orthop 2007;27:354-61. [Crossref] [PubMed]
- Karol LA, Johnston C, Mladenov K, et al. Pulmonary function following early thoracic fusion in non-neuromuscular scoliosis. J Bone Joint Surg Am 2008;90:1272-81. [Crossref] [PubMed]
- Jenks M, Craig J, Higgins J, et al. The MAGEC system for spinal lengthening in children with scoliosis: A NICE Medical Technology Guidance. Appl Health Econ Health Policy 2014;12:587-99. [Crossref] [PubMed]
- Rolton D, Richards J, Nnadi C. Magnetic controlled growth rods versus conventional growing rod systems in the treatment of early onset scoliosis: a cost comparison. Eur Spine J 2015;24:1457-61. [Crossref] [PubMed]
- Hosseini P, Pawelek J, Mundis GM, et al. Magnetically controlled growing rods for early-onset scoliosis: A multicenter study of 23 cases with minimum 2 years follow-up. Spine (Phila Pa 1976) 2016;41:1456-62. [Crossref] [PubMed]
- Teoh KH, Winson DM, James SH, et al. Do magnetic growing rods have lower complication rates compared with conventional growing rods? Spine J 2016;16:S40-4. [PubMed]
- Thompson W, Thakar C, Rolton DJ, et al. The use of magnetically-controlled growing rods to treat children with early-onset scoliosis: early radiological results in 19 children. Bone Joint J 2016;98-B:1240-7. [Crossref] [PubMed]
- Sankar WN, Skaggs DL, Yazici M, et al. Lengthening of dual growing rods and the law of diminishing returns. Spine (Phila Pa 1976) 2011;36:806-9. [Crossref] [PubMed]
- Roaf R. Vertebral growth and its mechanical control. J Bone Joint Surg Br 1960;42-B:40-59. [PubMed]
- R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. Available online: https://www.R-project.org/. 2016.
- Akbarnia BA, Breakwell LM, Marks DS, et al. Dual growing rod technique followed for three to eleven years until final fusion: the effect of frequency of lengthening. Spine (Phila Pa 1976) 2008;33:984-90. [Crossref] [PubMed]
- Cheung JP, Bow C, Samartzis D, et al. Frequent small distractions with a magnetically controlled growing rod for early-onset scoliosis and avoidance of the law of diminishing returns. J Orthop Surg (Hong Kong) 2016;24:332-7. [Crossref] [PubMed]
- Spurway AJ, Chukwunyerenwa CK, Kishta WE, et al. Sagittal Spine Length Measurement: A Novel Technique to Assess Growth of the Spine. Spine Deform 2016;4:331-7. [Crossref] [PubMed]
- Law M, Ma WK, Lau D, et al. Cumulative radiation exposure and associated cancer risk estimates for scoliosis patients: Impact of repetitive full spine radiography. Eur J Radiol 2016;85:625-8. [Crossref] [PubMed]
- de Onis M, Onyango AW, Borghi E, et al. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 2007;85:660-7. [Crossref] [PubMed]
- Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC Growth charts for the United States: methods and development. Vital Health Stat 11 2002;246:1-190. [PubMed]