Anterior cervical spine surgery-associated complications in a retrospective case-control study
Introduction
The anterior approach to the cervical spine constitutes a well-established surgical strategy, and one of the most commonly performed spinal procedures. Smith and Robinson (1) first described their technique for anterior cervical spine approach, while several modifications of this original technique have also been published (2). Anterior cervical approaches allow the efficient management of a variety of spinal pathology (3). They provide relatively easy access to the vertebral column, while their surgical outcome is satisfactory in the vast majority of cases (4). It would not be an overstatement that anterior cervical approach constitutes one of the most rewarding spinal procedures (4-12).
Despite the overall good outcome, various potential complications may occur on rare occasions (13-18). The majority of these complications are transient and self-limited, however in very rare instances, they may require a second surgical intervention, and if they remain undetected may even lead to death (17,19-27). It has been adequately demonstrated in the pertinent literature, that anterior cervical corpectomy and fusion (ACCF) procedures demonstrate higher complication rates than anterior cervical discectomy and fusions (ACDF) (27). Meticulous knowledge of all potential procedure-associated and postoperative complications is of paramount importance for their early recognition, and their proper management. Furthermore, identification of any complication-predisposing factors and situations may help avoid such complications, and in mitigating their overall clinical effect.
The purpose of our study was to evaluate the complication rate in anterior cervical spinal procedures in our institution, and identify the parameters that may predispose to their occurrence.
Methods
This is a retrospective, case-control study consisting of review of hospital charts by two residents (T.G., I.S.) separately, for any procedure-associated complications. Our study was approved by our Institutional Review Board. All the participants’ data handling was performed according to the Helsinki and the Health Insurance Portability and Accountability (HIPAA) acts. No participants’ informed consent was necessary for our retrospective study. The study covered a single institution, four attending neurosurgeons, over a 6-year period (January 2009 to December 2014).
All adult patients who underwent anterior spinal surgery in our institution were considered for eligibility in our study. Patients with previous anterior neck surgery for indications other than for spinal surgery were excluded. All patients underwent detailed neurological examination preoperatively, while their imaging work-up included cervical spine plain X-rays, and MRI. In specific cases, depending on the underlying pathology, the preoperative evaluation also included flexion/extension X-rays, CT scan, and EMG and nerve conduction velocity studies.
All anterior approaches were performed from the right side, under general endotracheal anesthesia, and fluoroscopic imaging. All ACDF procedures were performed with the Smith-Robinson technique. An allograft was used in all our cases. The procedures were performed under neurophysiological monitoring with motor and somato-sensory evoked potential (MEP & SSEP), as well as spontaneous electromyography monitoring. All patients with complications formed the case group, while the remaining patients served as the control group. Every patient was routinely re-evaluated with clinical examination at 1, 6, and 12 months after their discharge, and then on a yearly basis in our outpatient clinic, while radiographic evaluation was obtained by plain X-rays at 12 months postoperatively.
The charts of 114 consecutive patients undergoing anterior cervical spine surgery were reviewed. The patient’s gender and age, clinical presentation, diagnosis, type of surgery, and length of fusion were recorded and tested for their potential role as risk factors. The occurrence of any post-operative complications, their time of occurrence, the mode of treatment, and the outcome were also registered. Complications occurring during the initial 14 days were considered as perioperative, while the remaining as delayed.
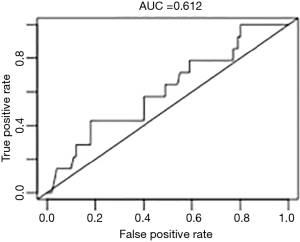
We used descriptive statistics to calculate the frequency for each observed complication in terms of absolute counts and percentages. Comparisons between groups were performed with the Chi-squared test (or Fisher’s exact test, if the number of observations was >6) after constructing contingency tables, and visualized by bar-plots. Continuous variables were summarized with the mean and their standard deviation, and were compared by using the Student’s t-test and boxplots. The level of statistical significance was defined by a P value <0.05. Potential risk factors were identified by means of univariate logistic regression (Wald’s P value <0.05). Odds ratios (ORs) are presented with 95% confidence intervals (CIs) and visualized with the OR plots. The predictive value of the logistic model was assessed and visualized by the area under the curve (AUC) of the receiver operating characteristics curve (ROC) of the logistic model. The statistical analysis was performed with the statistical environment R.
Results
Patients’ demographic and clinical data
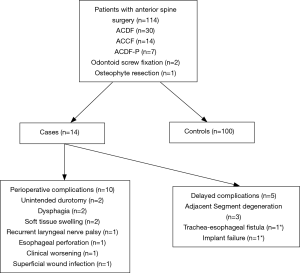
Our study population included 73 males and 41 females (Table 1, Figure 1). The patients’ age ranged between 21 and 82 years (mean, 49.92; SD, 14.25). Their preoperative diagnoses included both pathology of traumatic and degenerative etiology. More specifically, there were 27 trauma cases suffering from subluxation, vertebral body fracture, and/or traumatic intervertebral disc herniation, with or without myelopathy. The remaining 87 patients had pathology of degenerative etiology including cervical spondylosis, intervertebral disc protrusion/extrusion, radiculopathy, myelopathy, and Forestier’s disease. ACDF was the most commonly performed procedure in our series. The operative blood loss varied between 30 and 780 mL (mean, 130 mL). Their follow up period ranged from 6 to 78 months (mean, 42.5).

Full table
Complications
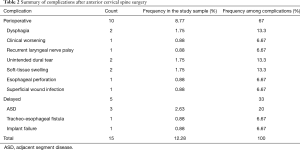
Fourteen patients (12.28%) developed post-operative complications and were included in the complication group. In ten patients (71.42%) the complications occurred at the early post-operative period, while in the remaining four (28.58%) the complications occurred later (Table 2, Figure 1).
Full table
Perioperative complications
The patients developing perioperative complications are summarized on Table 3 and Figure 1. Accidental dural penetration occurred in two patients (1.7%). In one case cerebrospinal (CSF) fistula developed postoperatively, which was treated with a lumbar drain insertion. In the other case, a lumbar drain was inserted after the completion of the procedure to prevent a CSF wound leakage. Both patients had no further consequences. Dysphagia was encountered in two patients (1.7%), and was spontaneously resolved within 7–10 days, postoperatively. Two patients (1.7%) developed a postoperative soft tissue hematoma within the first 24 postoperative hours, which presented with severe difficulty in swallowing. Both patients were closely observed, and their hematomas were spontaneously absorbed. Esophageal perforation was documented in one patient (0.9%), undergoing two-level ACDF for degenerative severe spondylosis and myelopathy. They presented with progressive hoarseness, dysphagia, and low-grade fever, and was confirmed with a CT scan, which showed air in the mediastinum. The patient had a second urgent operation, in which the esophageal wall perforation was corrected with a muscular patch. The patient was placed on parenteral alimentation and antibiotics for six weeks. He was finally discharged with no other problems. Symptomatic postoperative recurrent laryngeal nerve (RLN) palsy occurred in one patient (0.9%), presenting with severe hoarseness postoperatively, and the diagnosis was confirmed by using indirect laryngoscopy. Small doses of methyl-prednisolone were given for 5 days, and the patient’s symptomatology gradually resolved. In one case (0.9%) aggravation of a preexisting myelopathy was observed, with worsening of the patient’s neurological condition. The patient, who initially was treated with two-level ACDF for myelopathy of degenerative etiology, had to undergo a second procedure, which was a posterior decompression. His neurological condition progressively improved after the second procedure. It is worth noting that neuro-monitoring could not assist in preventing any of the observed perioperative complications.

Full table
Delayed complications
Four patients developed delayed complications (Table 4, Figure 1). Mechanical failure of the implanted instrumentation occurred in one case (0.9%). The patient had undergone a single-level (C7) corpectomy for a traumatic vertebral body fracture and subluxation. An anterior plate was implanted, and the patient underwent a 360° fusion in two settings. He returned approximately one year after his discharge, complaining of progressively worsening odynophagia, difficulty in swallowing, hoarseness, and low fever. His imaging work up including X-rays and CT scan demonstrated a tracheo-esophageal fistula, most probably secondary to a large neck abscess, while one of the inferior anterior cervical plate screws had been pulled out. The patient was taken to surgery to drain his abscess, and to remove the previously implanted cervical plate. He remained on antibiotics for a long period of time, and recovered with no further problems. Another patient (0.9%) developed a superficial surgical wound infection postoperatively, which was treated with oral antibiotics with no further consequences. Finally, adjacent intervertebral segment disc degeneration was documented in three patients (2.7%), who underwent a second ACDF procedure for managing their disease.

Full table
Risk factors
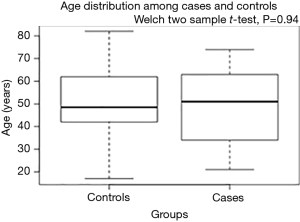
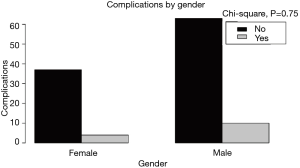
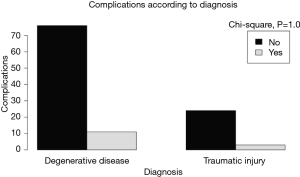
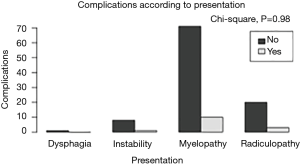
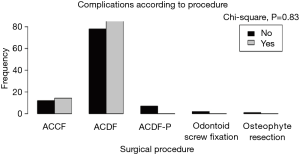
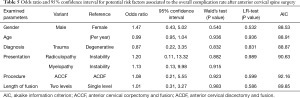
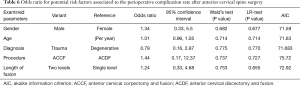
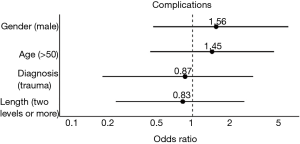
There were no statistically important differences between the case group and the control group in terms of the patients’ gender (P=0.75), age (P=0.94), clinical presentation (P=0.98), diagnosis (P=0.87), spinal procedure (P=0.83), and length of fusion (P=1) (Table 1, Figures 2-6). The available data permitted logistic regression analysis only for the overall complications and the perioperative ones. None of the above-mentioned parameters could be considered as a risk factor for postoperative complications according to the employed logistic regression (Tables 5,6, Figures 7,8).
Full table
Full table
Discussion
Summary of findings
The most important findings from the current study is that the cumulative incidence of postoperative complications after anterior spinal surgery is as high as 13.2%. Complications at the early postoperative period are more common and in most instances do not require surgical treatment, contrary to the delayed ones, where surgical intervention is required in most cases. Furthermore, we could not identify risk factors among the parameters tested.
Background
Anterior cervical spine surgery-associated complications are well described in the literature, even though their reported incidence widely varies among published series. Meticulous knowledge of any potential complications is of paramount importance for their early recognition, and their proper management. Moreover, actual incidence of anterior spinal procedure complications is of importance for medico-legal purposes. Underreporting of complications may generate the false impression that anterior cervical approaches have no complications, and may establish an erroneously legal background.
The long list of complications includes infection, abscess, and hematoma formation (20,26-29). Additionally, neurovascular or adjacent organ injuries have been reported (17,20,27,29-39). Implant related complications have also been reported in the literature (20,27,40-44). The list also includes functional complications such as dysphagia, dysphonia, and difficulty in swallowing (7,45-51). Although the vast majority of these complications are of minor clinical impact, there are extremely rare occasions that the outcome of a complication may be troublesome or even fatal.
Adjacent segment disc disease
The most common complication was the occurrence of adjacent intervertebral disc degeneration in 2.7% of our cases. Although adjacent intervertebral disc degeneration is not typically listed among the ACDF complications, it is well documented that anterior cervical spine surgery with fusion significantly alter the regional biomechanics, increase the load to the adjacent intervertebral discs, and introduce stress and instability to them (52-62). However, Hilibrand and Robbins (63) raised the question of whether this adjacent segment degeneration was the result of the previous surgical intervention or may just reflect the underlying natural history of the cervical degenerative process. Matsumoto et al. (64) found that patients with anterior fusion had a higher rate of radiographically proven adjacent segment degeneration. Nevertheless, recently published data showed that the incidence of adjacent segment degeneration after ACDF was 12.2%, and subsequently increased to 25% after a second cervical fusion (40,43). Similarly, Bohlman et al. (5) concluded that 9% of their patients developed adjacent segment disease within 6 years after ACDF, and 7.4% of them required a reoperation. Likewise, Hilibrand et al. (65) anticipated that more than 25% of patients undergoing ACDF will develop adjacent segment degeneration. They calculated that the annual incidence of adjacent segment degeneration is 2.9% per year (65).
Dysphagia
In the majority of the previously published series, dysphagia and dysphonia are the most common postoperative complications, with rates ranging from 1–79% (16,45). This wide variation may be partially explained by the fact that dysphagia is routinely underestimated as a complication (21,25,66). There are reports on the incidence of postoperative dysphagia based on the surgeon’s interpretation or the patient’s interpretation. Thus, Johns et al. (49) reported that the incidence of dysphagia was 11% when based on the physicians’ notes, while it was 57% when the patients were surveyed. According to Dettori et al. (67) a patient’s reported outcome has been shown to be more reliable, valid, and preferable. Dysphagia was observed in 1.7% of our patients, and this was based on patients’ reports. Khaki et al. (48) reported 52% incidence of postoperative dysphagia in patients undergoing anterior cervical spine surgery. It has been postulated that soft tissue swelling is the most common cause of postoperative dysphagia (2,16,68-70). However, there are studies supporting the theory that soft tissue swelling is not related to the development of postoperative dysphagia (46,48). Various causes have been implicated in the development of postoperative dysphagia, including RLN palsy, pharyngeal plexus denervation, esophageal direct injury, and regional esophageal ischemia (71-75). In addition, postoperative hematoma and scar tissue formation should be ruled out, especially in cases of chronic dysphagia (76). However, the underlying pathophysiology of postoperative dysphagia remains poorly understood (77). With all the existing controversies, the low dysphagia incidence observed in our study may be related to the relative low rate of anterior cervical plate usage, the application of solely manual retraction with periodic pressure release, and the careful intraoperative soft-tissue handling. In all our cases, dysphagia was transient and required no special treatment. Although most studies reported that dysphagia decreases with time, the prevalence of chronic dysphagia is more common than previously considered (73,78-80).
Postoperative hematoma
Postoperative wound hematoma occurred in 1.7% in our series. The reported incidence of postoperative wound hematoma among the previously published series is 0.2–2.4% (20,21,81-89). A postoperative hematoma although occurs rarely, it may potentially be a life-threatening complication. Generally, immediate recognition and evacuation of the hematoma is necessary, in order to avoid airway compromise. It is well known that the development of such a complication is more common in the acute postoperative period. It has to be emphasized however, that up to 35% of hematomas has been reported to be presented in a delayed fashion, at an average of 6 days postoperatively (28,32). Interestingly, O’Neil et al. (28) mentioned that in 27% of their cases a drain was in place, while in 27% of cases the hematoma formed shortly after the drain removal, raising significant questions regarding its role in preventing a postoperative hematoma. The importance of meticulous intraoperative hemostasis cannot be overemphasized. The role of a drain in preventing a hematoma formation remains to be defined.
Dural penetration
Intraoperative dural penetration was observed in 1.7% of our cases. Incidental durotomy is a rare, and potentially serious complication, which is reported with incidence varying between 0.2–0.5% (20,90). The reported incidence of meningitis secondary to CSF leak after anterior cervical spine surgery is approximately 0.2% (21). The employment of meticulous and careful, microscopic dissection during the posterior longitudinal ligament (PLL) opening, especially in chronic-standing disc extrusion cases, and/or in cases of ossified PLL is of paramount importance. Intraoperative recognition of the dural violation allows the proper management of any potential CSF leaks, and thus minimizes the risk of any postoperative infections.
Esophageal perforation
Esophageal perforation occurred in 0.9% of our cases. The overall incidence ranges between 0 and 3.4% (3,91-95). Fountas et al. (20) reported an incidence of 0.3% while Zhong et al. (33) reported 0.45%. Although the majority of patients suffering esophageal perforation have a good prognosis, this complication is still associated with mortality rates up to 16% (96). Interestingly, perforation of the esophagus after a previous anterior cervical procedure may occur as late as 10 years after surgery (36). Optimal treatment of esophageal perforation remains controversial. There are reports supporting a conservative management (19,97-100). However, the most preferable therapeutic strategy is immediate surgical repair (3,91,93,95,101-105). The importance of intraoperative or early recognition of this complication cannot be overemphasized. The risk of any esophageal injuries is higher in patients with previous neck surgeries, or neck irradiation.
Neurological complications
Worsening of preexisting myelopathy may occur in any spinal procedures. Its incidence in our series was 0.9%. Fountas et al. (20). have reported aggravation of preexisting myelopathy secondary to spinal cord contusion in 0.2% of their cases. It is well established that patients with pre-existing myelopathy have significantly higher incidence of procedure-associated complications (13.4%) and mortality rates (0.6%) compared with patients without myelopathy (6.3% and 0.1%, respectively) (29). Careful microscopic surgical technique and the employment of intraoperative electrophysiological monitoring may minimize the risk of worsening the patient’s preoperative neurological condition.
RLN palsy
Another common complication is RLN palsy. There are studies showing that RLN palsy is underreported (71,106). Dysphonia and/or hoarseness are the most common clinical expression of unilateral vocal paralysis, while bilateral RLN palsy can lead to respiratory insufficiency (23,107,108). In our series, the incidence of symptomatic RLN palsy was documented in 0.9% of our patients. It is documented that the incidence of spontaneous, asymptomatic, preoperative RLN palsy is approximately 1.6% (109,110). Jung et al. (111) noticed that the incidence of clinically symptomatic RLN palsy among patients undergoing anterior cervical spine surgery was 8.3% in the early postoperative period, while another 10.8% of their patients remained asymptomatic despite the presence of RLN paresis or paralysis. Similarly, Fountas et al. (20) reported 3.1% postoperative clinically symptomatic RLN palsy in their series. Contrariwise, Starmer et al. (50) found that postoperative vocal fold paralysis after anterior cervical disc surgery was only 0.1%. By anatomical point of view, the right RLN is more vulnerable to injury (112). Therefore a left-sided approach may be advantageous. Although the pathophysiology of RLN palsy remains ill defined, the avoidance of excessive mechanical retraction may minimize the risk of postoperative RLN paresis or palsy.
Implant failure
Implant and/or graft failure is another complication associated with anterior cervical spine surgery. The incidence of screw pullout was 0.9%, in our series. Cloward (113) provided one of the first reports on graft migration. Since then, mechanical failure and/or screw migration have been reported (41,42,97,114-116). Initial malposition or suboptimal position is the most common reason for mechanical fatigue, and eventual failure of the implant.
Surgical wound infection
Superficial or deep wound infections are included among the anterior cervical surgery complications. In our series, only 0.9% developed superficial wound infection. It has been demonstrated that the incidence of postoperative infections is strongly associated with the patients’ age. Veeravagu et al. (7) found that younger age was associated with increased risk of infection. They also found that postoperative surgical wound infection was the most common cause for readmission (7). The presence of co-morbidity may also increase the risk of a postoperative surgical wound infection (7). Boakye et al. (29), mentioned that patients aged 65–84 years were eight times more likely to have an adverse outcome. Likewise, Lovecchio et al. (26) also reported that certain preoperative factors, such as patient age over 65 and preoperative hospital stay more than 24 hours, conferred a significantly higher likelihood of a complication.
Cumulative complication rate
The cumulative complication rate in our series was 13.2%, while no deaths occurred. Fountas et al. (20), reported that the overall morbidity rate in their ACDF series was 19.3%, while the mortality rate was 0.1%. Similarly, Veeravagu et al. (7), estimated that the overall mortality at 2 years was 0.1% in the single level ACDF procedures, and 0.18% among their multilevel cases. Additionally, the complication rate was 2.1% for single level ACDFs, with overall complications more common in multilevel procedure. They also reported annual incidence of revision surgery in single and multilevel cases of 2.9% per year and 3.4% per year, respectively (7). Bilbao et al. (27) reported a complication rate of 25% in patients undergoing cervical spondylotic corpectomies. Extensive corpectomy procedures seem to be associated with higher complication rates (27).
Study limitations
It has to be emphasized that our study carries significant limitations and weaknesses. First of all, the current study is a retrospective one, thus carrying all biases of retrospective studies. Additionally, the limited size of our clinical series may compromise the statistical power of our results. Another potential problem is the inclusion of different type of anterior cervical spine procedures. However, the purpose of our study was to provide data of all anterior cervical spine procedures, and not only of a specific type, since many of the observed complications are associated with the anterior approach itself.
Conclusions
Anterior cervical spine procedures have been associated with quite satisfactory outcome in the vast majority of cases. However, the occurrence of troublesome complications, although rare, needs to be taken into consideration. We could not identify any modifiable preoperative risk factors to prevent any perioperative and/or delayed complications. Awareness, early recognition and appropriate management are of paramount importance for improving the outcome of these patients and their quality of life. Moreover, avoidance or mitigation of any complications may decrease the length of hospital stay, the number of hospitalre-admissions, thus significantly decreasing the overall health cost.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflict of interest to declare.
Ethical Statement: Our study was approved by our Institutional Review Board. All the participants’ data handling was performed according to the Helsinki and the Health Insurance Portability and Accountability (HIPAA) acts. No participants’ informed consent was necessary for our retrospective study
References
- Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 1958;40-A:607-24. [Crossref] [PubMed]
- Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg 1958;15:602-17. [Crossref] [PubMed]
- Newhouse KE, Lindsey RW, Clark CR, et al. Esophageal perforation following anterior cervical spine surgery. Spine (Phila Pa 1976) 1989;14:1051-3. [Crossref] [PubMed]
- Cloward RB. History of the anterior cervical fusion technique. J Neurosurg 1985;63:817-9. [PubMed]
- Bohlman HH, Emery SE, Goodfellow DB, et al. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am 1993;75:1298-307. [Crossref] [PubMed]
- Bekelis K, Desai A, Bakhoum SF, et al. A predictive model of complications after spine surgery: the National Surgical Quality Improvement Program (NSQIP) 2005-2010. Spine J 2014;14:1247-55. [Crossref] [PubMed]
- Veeravagu A, Cole T, Jiang B, et al. Revision rates and complication incidence in single- and multilevel anterior cervical discectomy and fusion procedures: an administrative database study. Spine J 2014;14:1125-31. [Crossref] [PubMed]
- Majd ME, Vadhva M, Holt RT. Anterior cervical reconstruction using titanium cages with anterior plating. Spine (Phila Pa 1976) 1999;24:1604-10. [Crossref] [PubMed]
- Hacker RJ, Cauthen JC, Gilbert TJ, et al. A prospective randomized multicenter clinical evaluation of an anterior cervical fusion cage. Spine (Phila Pa 1976) 2000;25:2646-54; discussion 2655. [Crossref] [PubMed]
- Wang JC, McDonough PW, Endow KK, et al. Increased fusion rates with cervical plating for two-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2000;25:41-5. [Crossref] [PubMed]
- Samartzis D, Shen FH, Matthews DK, et al. Comparison of allograft to autograft in multilevel anterior cervical discectomy and fusion with rigid plate fixation. Spine J 2003;3:451-9. [Crossref] [PubMed]
- Papadopoulos EC, Huang RC, Girardi FP, et al. Three-level anterior cervical discectomy and fusion with plate fixation: radiographic and clinical results. Spine (Phila Pa 1976) 2006;31:897-902. [Crossref] [PubMed]
- Clements DH, O'Leary PF. Anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 1990;15:1023-5. [Crossref] [PubMed]
- Bose B. Anterior cervical fusion using Caspar plating: analysis of results and review of the literature. Surg Neurol 1998;49:25-31. [Crossref] [PubMed]
- Stewart M, Johnston RA, Stewart I, et al. Swallowing performance following anterior cervical spine surgery. Br J Neurosurg 1995;9:605-9. [Crossref] [PubMed]
- Daniels AH, Riew KD, Yoo JU, et al. Adverse events associated with anterior cervical spine surgery. J Am Acad Orthop Surg 2008;16:729-38. [Crossref] [PubMed]
- Campbell PG, Yadla S, Malone J, et al. Early complications related to approach in cervical spine surgery: single-center prospective study. World Neurosurg 2010;74:363-8. [Crossref] [PubMed]
- Fehlings MG, Smith JS, Kopjar B, et al. Perioperative and delayed complications associated with the surgical treatment of cervical spondylotic myelopathy based on 302 patients from the AOSpine North America Cervical Spondylotic Myelopathy Study. J Neurosurg Spine 2012;16:425-32. [Crossref] [PubMed]
- Woolley SL, Smith DR. Pharyngeal perforation: a late complication of cervical spine surgery. J Laryngol Otol 2005;119:913-6. [Crossref] [PubMed]
- Fountas KN, Kapsalaki EZ, Nikolakakos LG, et al. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976) 2007;32:2310-7. [Crossref] [PubMed]
- Bertalanffy H, Eggert HR. Complications of anterior cervical discectomy without fusion in 450 consecutive patients. Acta Neurochir (Wien) 1989;99:41-50. [Crossref] [PubMed]
- Fielding JW. Complications of anterior cervical disk removal and fusion. Clin Orthop Relat Res 1992.10-3. [PubMed]
- Flynn TB. Neurologic complications of anterior cervical interbody fusion. Spine (Phila Pa 1976) 1982;7:536-9. [Crossref] [PubMed]
- Taylor BA, Vaccaro A, Albert TJ. Complications of anterior and posterior surgical approaches in the treatment of cervical degenerative disc disease. Semin Spine Surg 1999;11:337-46.
- Tew JM, Mayfield FH. Complications of surgery of the anterior cervical spine. Clin Neurosurg 1976;23:424-34. [PubMed]
- Lovecchio F, Hsu WK, Smith TR, et al. Predictors of thirty-day readmission after anterior cervical fusion. Spine (Phila Pa 1976) 2014;39:127-33. [Crossref] [PubMed]
- Bilbao G, Duart M, Aurrecoechea JJ, et al. Surgical results and complications in a series of 71 consecutive cervical spondylotic corpectomies. Acta Neurochir (Wien) 2010;152:1155-63. [Crossref] [PubMed]
- O'Neill KR, Neuman B, Peters C, et al. Risk factors for postoperative retropharyngeal hematoma after anterior cervical spine surgery. Spine (Phila Pa 1976) 2014;39:E246-52. [Crossref] [PubMed]
- Boakye M, Patil C, Santarelli J, et al. Cervical spondylotic myelopathy: complications and outcomes after spinal fusion. Neurosurgery 2008;62:455-61. [Crossref] [PubMed]
- Loret JE, Francois P, Papagiannaki C, et al. Internal carotid artery dissection after anterior cervical disc replacement: first case report and literature review of vascular complications of the approach. Eur J Orthop Surg Traumatol 2013;23 Suppl 1:S107-10. [Crossref] [PubMed]
- Park HK, Jho HD. The management of vertebral artery injury in anterior cervical spine operation: a systematic review of published cases. Eur Spine J 2012;21:2475-85. [Crossref] [PubMed]
- Yu NH, Jahng TA, Kim CH, et al. Life-threatening late hemorrhage due to superior thyroid artery dissection after anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2010;35:E739-42. [Crossref] [PubMed]
- Zhong ZM, Jiang JM, Qu DB, et al. Esophageal perforation related to anterior cervical spinal surgery. J Clin Neurosci 2013;20:1402-5. [Crossref] [PubMed]
- Rath GP, Marda M, Sokhal N, et al. Hypopharyngeal injury leading to subcutaneous emphysema after anterior cervical discectomy and artificial cervical disc placement. J Clin Neurosci 2010;17:1447-9. [Crossref] [PubMed]
- Palumbo MA, Aidlen JP, Daniels AH, et al. Airway compromise due to laryngopharyngeal edema after anterior cervical spine surgery. J Clin Anesth 2013;25:66-72. [Crossref] [PubMed]
- Nourbakhsh A, Garges KJ. Esophageal perforation with a locking screw: a case report and review of the literature. Spine (Phila Pa 1976) 2007;32:E428-35. [Crossref] [PubMed]
- Sansur CA, Early S, Reibel J, et al. Pharyngocutaneous fistula after anterior cervical spine surgery. Eur Spine J 2009;18:586-91. [Crossref] [PubMed]
- Guerin P, El Fegoun AB, Obeid I, et al. Incidental durotomy during spine surgery: incidence, management and complications. A retrospective review. Injury 2012;43:397-401. [Crossref] [PubMed]
- Syre P, Bohman LE, Baltuch G, et al. Cerebrospinal fluid leaks and their management after anterior cervical discectomy and fusion: a report of 13 cases and a review of the literature. Spine (Phila Pa 1976) 2014;39:E936-43. [Crossref] [PubMed]
- Bydon M, Xu R, Macki M, et al. Adjacent segment disease after anterior cervical discectomy and fusion in a large series. Neurosurgery 2014;74:139-46; discussion 146. [Crossref] [PubMed]
- Gazzeri R, Tamorri M, Faiola A, et al. Delayed migration of a screw into the gastrointestinal tract after anterior cervical spine plating. Spine (Phila Pa 1976) 2008;33:E268-71. [Crossref] [PubMed]
- Fountas KN, Kapsalaki EZ, Machinis T, et al. Extrusion of a screw into the gastrointestinal tract after anterior cervical spine plating. J Spinal Disord Tech 2006;19:199-203. [Crossref] [PubMed]
- Xu R, Bydon M, Macki M, et al. Adjacent segment disease after anterior cervical discectomy and fusion: clinical outcomes after first repeat surgery versus second repeat surgery. Spine (Phila Pa 1976) 2014;39:120-6. [Crossref] [PubMed]
- Bhatia NN. Long-Term Outcomes and Complications Following Anterior and Posterior Cervical Spine Surgery. Seminars in Spine Surgery 2009;21:177-84. [Crossref]
- Riley LH, Vaccaro AR, Dettori JR, et al. Postoperative dysphagia in anterior cervical spine surgery. Spine (Phila Pa 1976) 2010;35:S76-85. [Crossref] [PubMed]
- Kepler CK, Rihn JA, Bennett JD, et al. Dysphagia and soft-tissue swelling after anterior cervical surgery: a radiographic analysis. Spine J 2012;12:639-44. [Crossref] [PubMed]
- Danto J, DiCapua J, Nardi D, et al. Multiple cervical levels: increased risk of dysphagia and dysphonia during anterior cervical discectomy. J Neurosurg Anesthesiol 2012;24:350-5. [Crossref] [PubMed]
- Khaki F, Zusman NL, Nemecek AN, et al. Postoperative prevertebral soft tissue swelling does not affect the development of chronic dysphagia following anterior cervical spine surgery. Spine (Phila Pa 1976) 2013;38:E528-32. [Crossref] [PubMed]
- Johns MM, Whitesides TE. Dysphagia following anterior cervical spine surgery. Semin Spine Surg 2004;16:274-8. [Crossref]
- Starmer HM, Riley LH, Hillel AT, et al. Dysphagia, short-term outcomes, and cost of care after anterior cervical disc surgery. Dysphagia 2014;29:68-77. [Crossref] [PubMed]
- Joaquim AF, Murar J, Savage JW, et al. Dysphagia after anterior cervical spine surgery: a systematic review of potential preventative measures. Spine J 2014;14:2246-60. [Crossref] [PubMed]
- Eck JC, Humphreys SC, Lim TH, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976) 2002;27:2431-4. [Crossref] [PubMed]
- Javedan SP, Dickman CA. Cause of adjacent-segment disease after spinal fusion. Lancet 1999;354:530-1. [Crossref] [PubMed]
- DiAngelo DJ, Foley KT, Morrow BR, et al. In vitro biomechanics of cervical disc arthroplasty with the ProDisc-C total disc implant. Neurosurg Focus 2004;17:E7. [Crossref] [PubMed]
- Kowalczyk I, Lazaro BC, Fink M, et al. Analysis of in vivo kinematics of 3 different cervical devices: Bryan disc, ProDisc-C, and Prestige LP disc. J Neurosurg Spine 2011;15:630-5. [Crossref] [PubMed]
- Matsunaga S, Kabayama S, Yamamoto T, et al. Strain on intervertebral discs after anterior cervical decompression and fusion. Spine (Phila Pa 1976) 1999;24:670-5. [Crossref] [PubMed]
- McAfee PC, Cunningham BW, Hayes V, et al. Biomechanical analysis of rotational motions after disc arthroplasty: implications for patients with adult deformities. Spine (Phila Pa 1976) 2006;31:S152-60. [Crossref] [PubMed]
- Prasarn ML, Baria D, Milne E, et al. Adjacent-level biomechanics after single versus multilevel cervical spine fusion. J Neurosurg Spine 2012;16:172-7. [Crossref] [PubMed]
- Puttlitz CM, Rousseau MA, Xu Z, et al. Intervertebral disc replacement maintains cervical spine kinetics. Spine (Phila Pa 1976) 2004;29:2809-14. [Crossref] [PubMed]
- Rihn JA, Lawrence J, Gates C, et al. Adjacent segment disease after cervical spine fusion. Instr Course Lect 2009;58:747-56. [PubMed]
- Nunley PD, Jawahar A, Kerr EJ, et al. Factors affecting the incidence of symptomatic adjacent-level disease in cervical spine after total disc arthroplasty: 2- to 4-year follow-up of 3 prospective randomized trials. Spine (Phila Pa 1976) 2012;37:445-51. [Crossref] [PubMed]
- Terai T, Faizan A, Sairyo K, et al. Operated and adjacent segment motions for fusion versus cervical arthroplasty: a pilot study. Clin Orthop Relat Res 2011;469:682-7. [Crossref] [PubMed]
- Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J 2004;4:190S-4S. [Crossref] [PubMed]
- Matsumoto M, Okada E, Ichihara D, et al. Anterior cervical decompression and fusion accelerates adjacent segment degeneration: comparison with asymptomatic volunteers in a ten-year magnetic resonance imaging follow-up study. Spine (Phila Pa 1976) 2010;35:36-43. [Crossref] [PubMed]
- Hilibrand AS, Carlson GD, Palumbo MA, et al. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 1999;81:519-28. [Crossref] [PubMed]
- Edwards CC, Karpitskaya Y, Cha C, et al. Accurate identification of adverse outcomes after cervical spine surgery. J Bone Joint Surg Am 2004;86-A:251-6. [Crossref] [PubMed]
- Dettori L CJ, Hanson B, Norvell DC. Clinician based outcomes measures. In: Chapman JR, Hanson BP, Dettori JR, editors. Spine outcomes measures and instruments. Thieme 1st ed: Thieme, 2007.
- Chang SW, Kakarla UK, Maughan PH, et al. Four-level anterior cervical discectomy and fusion with plate fixation: radiographic and clinical results. Neurosurgery 2010;66:639-46; discussion 646-7. [Crossref] [PubMed]
- Martin RE, Neary MA, Diamant NE. Dysphagia following anterior cervical spine surgery. Dysphagia 1997;12:2-8; discussion 9-10. [Crossref] [PubMed]
- Frempong-Boadu A, Houten JK, Osborn B, et al. Swallowing and speech dysfunction in patients undergoing anterior cervical discectomy and fusion: a prospective, objective preoperative and postoperative assessment. J Spinal Disord Tech 2002;15:362-8. [Crossref] [PubMed]
- Netterville JL, Koriwchak MJ, Winkle M, et al. Vocal fold paralysis following the anterior approach to the cervical spine. Ann Otol Rhinol Laryngol 1996;105:85-91. [Crossref] [PubMed]
- Morpeth JF, Williams MF. Vocal fold paralysis after anterior cervical diskectomy and fusion. Laryngoscope 2000;110:43-6. [Crossref] [PubMed]
- Bazaz R, Lee MJ, Yoo JU. Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine (Phila Pa 1976) 2002;27:2453-8. [Crossref] [PubMed]
- Heese O, Schröder F, Westphal M, et al. Intraoperative measurement of pharynx/esophagus retraction during anterior cervical surgery. Part I: pressure. Eur Spine J 2006;15:1833-7. [Crossref] [PubMed]
- Heese O, Fritzsche E, Heiland M, et al. Intraoperative measurement of pharynx/esophagus retraction during anterior cervical surgery. Part II: perfusion. Eur Spine J 2006;15:1839-43. [Crossref] [PubMed]
- Ebraheim NA, DeTroye RJ, Rupp RE, et al. Osteosynthesis of the cervical spine with an anterior plate. Orthopedics 1995;18:141-7. [PubMed]
- Rihn JA, Kane J, Albert TJ, et al. What is the incidence and severity of dysphagia after anterior cervical surgery? Clin Orthop Relat Res 2011;469:658-65. [Crossref] [PubMed]
- Lee MJ, Bazaz R, Furey CG, et al. Risk factors for dysphagia after anterior cervical spine surgery: a two-year prospective cohort study. Spine J 2007;7:141-7. [Crossref] [PubMed]
- Smith-Hammond CA, New KC, Pietrobon R, et al. Prospective analysis of incidence and risk factors of dysphagia in spine surgery patients: comparison of anterior cervical, posterior cervical, and lumbar procedures. Spine (Phila Pa 1976) 2004;29:1441-6. [Crossref] [PubMed]
- Kalb S, Reis MT, Cowperthwaite MC, et al. Dysphagia after anterior cervical spine surgery: incidence and risk factors. World Neurosurg 2012;77:183-7. [Crossref] [PubMed]
- Dohn DF. Anterior interbody fusion for treatment of cervical-disk conditions. JAMA 1966;197:897-900. [Crossref] [PubMed]
- Espersen JO, Buhl M, Eriksen EF, et al. Treatment of cervical disc disease using Cloward's technique. Acta Neurochirurgica 1984;70:97-114. [Crossref] [PubMed]
- Lunsford LD, Bissonette DJ, Zorub DS. Anterior surgery for cervical disc disease. Part 2: Treatment of cervical spondylotic myelopathy in 32 cases. J Neurosurg 1980;53:12-9. [Crossref] [PubMed]
- Hankinson HL, Wilson CB. Use of the operating microscope in anterior cervical discectomy without fusion. J Neurosurg 1975;43:452-6. [Crossref] [PubMed]
- Jacobs B, Krueger EG, Leivy DM. Cervical spondylosis with radiculopathy. Results of anterior diskectomy and interbody fusion. JAMA 1970;211:2135-9. [Crossref] [PubMed]
- Lunsford LD, Bissonette DJ, Jannetta PJ, et al. Anterior surgery for cervical disc disease. Part 1: Treatment of lateral cervical disc herniation in 253 cases. J Neurosurg 1980;53:1-11. [Crossref] [PubMed]
- Mosdal C. Cervical osteochondrosis and disc herniation. Eighteen years' use of interbody fusion by Cloward's technique in 755 cases. Acta Neurochir (Wien) 1984;70:207-25. [Crossref] [PubMed]
- Williams JL, Allen MB, Harkess JW. Late results of cervical discectomy and interbody fusion: some factors influencing the results. J Bone Joint Surg Am 1968;50:277-86. [Crossref] [PubMed]
- Wilson DH, Campbell DD. Anterior cervical discectomy without bone graft. Report of 71 cases. J Neurosurg 1977;47:551-5. [Crossref] [PubMed]
- Wang MC, Chan L, Maiman DJ, et al. Complications and mortality associated with cervical spine surgery for degenerative disease in the United States. Spine (Phila Pa 1976) 2007;32:342-7. [Crossref] [PubMed]
- Gaudinez RF, English GM, Gebhard JS, et al. Esophageal perforations after anterior cervical surgery. J Spinal Disord 2000;13:77-84. [Crossref] [PubMed]
- Graham JJ. Complications of cervical spine surgery. A five-year report on a survey of the membership of the Cervical Spine Research Society by the Morbidity and Mortality Committee. Spine (Phila Pa 1976) 1989;14:1046-50. [Crossref] [PubMed]
- Orlando ER, Caroli E, Ferrante L. Management of the cervical esophagus and hypofarinx perforations complicating anterior cervical spine surgery. Spine (Phila Pa 1976) 2003;28:E290-5. [Crossref] [PubMed]
- Romano PS, Campa DR, Rainwater JA. Elective cervical discectomy in California: postoperative in-hospital complications and their risk factors. Spine (Phila Pa 1976) 1997;22:2677-92. [Crossref] [PubMed]
- Vrouenraets BC, Been HD, Brouwer-Mladin R, et al. Esophageal perforation associated with cervical spine surgery: report of two cases and review of the literature. Dig Surg 2004;21:246-9. [Crossref] [PubMed]
- Brinster CJ, Singhal S, Lee L, et al. Evolving options in the management of esophageal perforation. Ann Thorac Surg 2004;77:1475-83. [Crossref] [PubMed]
- Chataigner H, Gangloff S, Onimus M. Spontaneous elimination by the natural tracts of screws of anterior cervical osteosynthesis. Apropos of a case. Rev Chir Orthop Reparatrice Appar Mot 1997;83:78-82. [PubMed]
- Kelly MF, Spiegel J, Rizzo KA, et al. Delayed pharyngoesophageal perforation: a complication of anterior spine surgery. Ann Otol Rhinol Laryngol 1991;100:201-5. [Crossref] [PubMed]
- Balmaseda MT, Pellioni DJ. Esophagocutaneous fistula in spinal cord injury: a complication of anterior cervical fusion. Arch Phys Med Rehabil 1985;66:783-4. [PubMed]
- Konstantakos AK, Temes RT. Delayed esophageal perforation: a complication of anterior cervical spine fixation. Ann Thorac Surg 2005;80:349. [Crossref] [PubMed]
- Haku T, Okuda S, Kanematsu F, et al. Repair of cervical esophageal perforation using longus colli muscle flap: a case report of a patient with cervical spinal cord injury. Spine J 2008;8:831-5. [Crossref] [PubMed]
- Ahn SH, Lee SH, Kim ES, et al. Successful repair of esophageal perforation after anterior cervical fusion for cervical spine fracture. J Clin Neurosci 2011;18:1374-80. [Crossref] [PubMed]
- Fuji T, Kuratsu S, Shirasaki N, et al. Esophagocutaneous fistula after anterior cervical spine surgery and successful treatment using a sternocleidomastoid muscle flap. A case report. Clin Orthop Relat Res 1991.8-13. [PubMed]
- Benazzo M, Spasiano R, Bertino G, et al. Sternocleidomastoid muscle flap in esophageal perforation repair after cervical spine surgery: concepts, techniques, and personal experience. J Spinal Disord Tech 2008;21:597-605. [Crossref] [PubMed]
- van Berge Henegouwen DP, Roukema JA, de Nie JC, et al. Esophageal perforation during surgery on the cervical spine. Neurosurgery 1991;29:766-8. [Crossref] [PubMed]
- Winslow CP, Meyers AD. Otolaryngologic complications of the anterior approach to the cervical spine. Am J Otolaryngol 1999;20:16-27. [Crossref] [PubMed]
- Kriskovich MD, Apfelbaum RI, Haller JR. Vocal fold paralysis after anterior cervical spine surgery: incidence, mechanism, and prevention of injury. Laryngoscope 2000;110:1467-73. [Crossref] [PubMed]
- Weisberg NK, Spengler DM, Netterville JL. Stretch-induced nerve injury as a cause of paralysis secondary to the anterior cervical approach. Otolaryngol Head Neck Surg 1997;116:317-26. [Crossref] [PubMed]
- Curley JW, Timms MS. Incidence of abnormality in routine 'vocal cord checks'. J Laryngol Otol 1989;103:1057-8. [Crossref] [PubMed]
- François JM, Castagnera L, Carrat X, et al. A prospective study of ENT complication following surgery of the cervical spine by the anterior approach (preliminary results). Rev Laryngol Otol Rhinol (Bord) 1998;119:95-100. [PubMed]
- Jung A, Schramm J. How to reduce recurrent laryngeal nerve palsy in anterior cervical spine surgery: a prospective observational study. Neurosurgery 2010;67:10-5; discussion 15. [Crossref] [PubMed]
- Lu J, Ebraheim NA, Nadim Y, et al. Anterior approach to the cervical spine: surgical anatomy. Orthopedics 2000;23:841-5. [PubMed]
- Cloward RB. Complications of anterior cervical disc operation and their treatment. Surgery 1971;69:175-82. [PubMed]
- Yen CP, Hwang TY, Wang CJ, et al. Fracture of anterior cervical plate implant--report of two cases. Acta Neurochir (Wien) 2005;147:665-7; discussion 667. [Crossref] [PubMed]
- Yee GK, Terry AF. Esophageal penetration by an anterior cervical fixation device. A case report. Spine (Phila Pa 1976) 1993;18:522-7. [Crossref] [PubMed]
- Pompili A, Canitano S, Caroli F, et al. Asymptomatic esophageal perforation caused by late screw migration after anterior cervical plating: report of a case and review of relevant literature. Spine (Phila Pa 1976) 2002;27:E499-502. [Crossref] [PubMed]


