Focal hypermobility observed in cervical arthroplasty with Mobi-C
Introduction
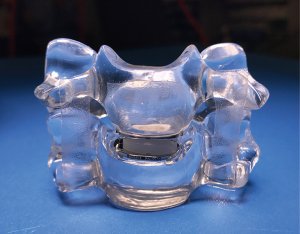
Cervical disc disease describes several symptomatic conditions resulting from intervertebral disc (IVD) degeneration. These include herniation, intervertebral foraminal stenosis and spondylosis, often causing compressive neurological pathologies such as radiculopathy and/or myelopathy (1,2). During recent years, there has been an increased interest in Cervical Total Disc Replacement (CTDR), due to a paradigm shift towards motion sparing technology. CTDR aims to restore disc height and preserve intervertebral motion following nerve decompression. Since the first CTDR device there have been several generations of design modification. One of the more recent designs has been the Mobi-C cervical artificial disc (LDR Medical; Troyes, France), seen in Figure 1. This device contains two endplates with lateral teeth for stability, and a mobile ultra-high molecular weight polyethylene (UHMWPE) core which repositions in response to movement of the superior plate. Early 6 months retrospective data on 23 patients, showed preserved ROM, and decreased VAS pain scores (3). Furthermore, Beaurain et al. (4) reported decreased NDI scores and VAS pain scores for the arm and neck 24 months postoperatively. Recent FDA Investigative Device Exemption studies have found that for both one level and two level operations, CTDR with the Mobi-C cervical artificial disc is a statistically superior or non-inferior procedure compared to anterior cervical discectomy and fusion (ACDF), in terms of key clinical and radiographic outcomes (5,6). The current paper reports on two cases of abnormal hypermobility observed in patients receiving CTDR with the Mobi-C cervical artificial disc. To our knowledge, such hypermobility has not been previously reported in the literature, with this device.
Case presentation
Case 1
A 55-year-old female presented with neck and arm pain and paraesthesia worsening over a 3-year time period. Imaging revealed multilevel foraminal stenosis and disc/osteophyte complex at C5/6 and C6/7. Decision and consent was completed for a C5/6 ACDF and C6/7 CTDR with the Mobi-C cervical artificial disc. A standard anterior approach via retraction of the musculo-visceral column was achieved to expose the appropriate levels. A Caspar distractor was used to distract the disc space at C6/7 and C5/6. A discectomy was performed and the posterior longitudinal ligament (PLL) was identified and resected, with decompression of the C6 and C7 nerves. A 6.5 mm Centinel (USA) Cage was implanted at C5/6 and a 5 mm height by 15 mm × 19 mm Mobi-C implant was inserted at C6/7. There were no intraoperative complications and blood loss was minimal (<20 cc). The patient was required to wear a soft collar and use anti-inflammatory medication for two weeks postoperatively.
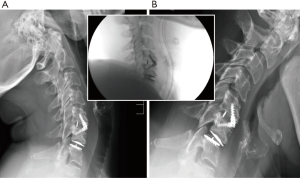
Intraoperative implant placement and vertebral alignment was within surgical guidelines (Figure 2). Flexion/extension radiographs taken at 3 months show focal hypermobility with 12° of motion and marked anterolisthesis on flexion (Figure 2). This had no negative influence on the clinical outcome, with the patient having sustained relief of her symptoms at the 18 months follow-up point.
Case 2
A 47-year-old female presented with bilateral C6 radiculopathy due to a disc/osteophyte complex. Attempts at conservative management were tried for a year including physical therapy, pain management therapy, non-steroidal anti-inflammatory medications/cortisone injections. The patient underwent a C5/6 CTDR with Mobi-C. A 5 mm height by 17 mm × 15 mm LDR Mobi-C cervical artificial disc was inserted at C5/6. There were no intraoperative complications and blood loss was minimal (<10 cc). The patient was required to wear a soft collar and use anti-inflammatory medication for two weeks postoperatively.
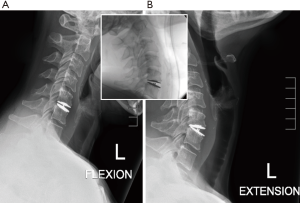
Flexion/extension radiographs taken at 6 weeks show extensive focal hypermobility on extension with 15.6° of motion (Figure 3). This excessive movement in hyperextension and ‘fish-mouth’ deformity had no negative influence on patient clinical outcomes, with the patient reporting complete alleviation of preoperative pain and continues to do well after 24 months postoperative.
Discussion
There are few reported cases of hypermobility in the literature. Case reports exist outlining cases of hypermobility with the M6-C and PCM devices (7,8). To our knowledge, this is the first reported instance of focal hypermobility with the LDR Mobi-C cervical artificial disc. The design of the Mobi-C cervical artificial disc relies upon a mobile UHMWPE core that can reposition over an inferior endplate in response to movement of the superior endplate. What appears to be happening in these two case studies is excessive core translation which corresponds to a large range of motion between the two endplates of the device. In Case 1 this appears to have coincided with minor posterior migration of the inferior device endplate.
Potential causes for this hypermobility arises from resection of the supporting ligaments during implantation. Excessive hypermobility during flexion, as seen in Case 1, could be a result of removal of the PLL, which is performed during cervical discectomy to ensure complete canal and exit foraminal decompression. Studies conducted by McAfee et al. (9) and Yu et al. (10), have shown that the PLL contributes towards the balance and stability of the cervical spine, naturally resisting excessive flexion. As such, they recommend that, where it does not interfere with nerve decompression, the PLL should be preserved during cervical spine surgery. This argument is counter-productive for CTDR surgery. However, as the goal is to decompress the neurological elements, and PLL resection is accepted as an important aspect of this surgery to confirm decompression.
The hypermobility during extension observed in Case 2 is caused by the resection of the anterior longitudinal ligament (ALL) which covers the anterior surface of the vertebral column, resisting excessive extension. Studies of the lumbar spine have shown the anterior longitudinal ligament is important in the biomechanics of the spine, resisting hypermobility, anterior migration and excessive facet joint loading following lumbar arthroplasty (11-13). However, for the cervical spine, ALL removal is essential to performing the discectomy as other structures such as the vertebral artery and spinal cord prevent alternative approaches. As such, perhaps it is valuable for surgeons to consider and investigate potential artificial reconstruction of the anterior longitudinal ligament with CTDR.
The key issue with such hypermobility is the fear that it will cause increased stress loading on the facet joints, accelerating their degeneration. This has been well known as an addition cause of pain in both the neck and lower back (14,15). As such hypermobility could result in such patients returning with additional pathologies in the future, an undesirable long-term outcome for a surgical procedure.
Conclusions
Cervical arthroplasty, as a technique, has advanced tremendously since its first use. While improvements have been made with each generation, as seen in this case study there are still complications which arise. Here we have reported two cases of focal hypermobility following CTDR with the LDR device, the Mobi-C cervical artificial disc. While both patients remained asymptomatic during follow-up, the potential for accelerated facet joint degeneration remains a concern. Potential preventative measures include preservation of the PLL and replacement of the ALL with an artificial substitute.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
References
- McAfee PC. The indications for lumbar and cervical disc replacement. Spine J 2004;4:177S-81S. [Crossref] [PubMed]
- Russell EJ. Cervical disk disease. Radiology 1990;177:313-25. [Crossref] [PubMed]
- Kim SH, Shin HC, Shin DA, et al. Early clinical experience with the mobi-C disc prosthesis. Yonsei Med J 2007;48:457-64. [Crossref] [PubMed]
- Beaurain J, Bernard P, Dufour T, et al. Intermediate clinical and radiological results of cervical TDR (Mobi-C) with up to 2 years of follow-up. Eur Spine J 2009;18:841-50. [Crossref] [PubMed]
- Davis RJ, Nunley PD, Kim KD, et al. Two-level total disc replacement with Mobi-C cervical artificial disc versus anterior discectomy and fusion: a prospective, randomized, controlled multicenter clinical trial with 4-year follow-up results. J Neurosurg Spine 2015;22:15-25. [Crossref] [PubMed]
- Hisey MS, Bae HW, Davis R, et al. Multi-center, prospective, randomized, controlled investigational device exemption clinical trial comparing Mobi-C Cervical Artificial Disc to anterior discectomy and fusion in the treatment of symptomatic degenerative disc disease in the cervical spine. Int J Spine Surg 2014.8. [PubMed]
- Gautschi OP, Corniola MV, Stienen MN, et al. Postoperative segmental hypermobility after cervical arthroplasty: A possible pathomechanism for outcome failure. J Clin Neurosci 2015;22:1194-6. [Crossref] [PubMed]
- Jadik S, Miller FC, Pietila AT. Cervical Arthroplasty with the M6-C Artificial Disc in Degenerative Disc Disease of the Cervical Spine. Archives of Medicine 2015;7:13.
- McAfee PC, Cunningham B, Dmitriev A, et al. Cervical disc replacement-porous coated motion prosthesis: a comparative biomechanical analysis showing the key role of the posterior longitudinal ligament. Spine (Phila Pa 1976) 2003;28:S176-85. [Crossref] [PubMed]
- Yu CC, Hao DJ, Ma YL, et al. The Role of Posterior Longitudinal Ligament in Cervical Disc Replacement: An Ovine Cadaveric Biomechanical Analysis. Med Sci Monit 2016;22:1843-9. [Crossref] [PubMed]
- Denozière G, Ku DN. Biomechanical comparison between fusion of two vertebrae and implantation of an artificial intervertebral disc. J Biomech 2006;39:766-75. [Crossref] [PubMed]
- Marchi L, Oliveira L, Coutinho E, et al. The importance of the anterior longitudinal ligament in lumbar disc arthroplasty: 36-Month follow-up experience in extreme lateral total disc replacement. Int J Spine Surg 2012;6:18-23. [Crossref] [PubMed]
- Rundell SA, Auerbach JD, Balderston RA, et al. Total disc replacement positioning affects facet contact forces and vertebral body strains. Spine (Phila Pa 1976) 2008;33:2510-7. [Crossref] [PubMed]
- Lewinnek GE, Warfield CA. Facet joint degeneration as a cause of low back pain. Clin Orthop Relat Res 1986.216-22. [PubMed]
- Manchikanti L, Singh V, Rivera J, et al. Prevalence of cervical facet joint pain in chronic neck pain. Pain Physician 2002;5:243-9. [PubMed]


