Outcomes and complications of S2 alar iliac fixation technique in patients with neuromuscular scoliosis: experience in a third level pediatric hospital
Introduction
Spinal deformities, especially scoliosis, are common in patients with cerebral palsy (CP). Its incidence is estimated to be around 20%, and varies according to the extent and severity of the neurological involvement. In non-ambulatory children with CP, the incidence of spinal deformities is reported by 62%, and up to 100% in children with greater neurological compromise in which this deformity might be extended caudally generating pelvic obliquity. This can result in imbalance in the coronal and sagittal planes (1,2).
Neuromuscular scoliosis differs from idiopathic scoliosis in several aspects. Neuromuscular scoliosis is characterized by further progression and rigidity of the deformity, early onset of the curves, and conservative treatments with brace are poorly tolerated and ineffective. In addition, there is a higher rate of postoperative complications mainly due to associated comorbidities (1,3,4). The main goals of surgical treatment of patients with neuromuscular scoliosis are maintaining posture in the seated position by leveling the pelvis, and to facilitate hygiene (5).
The literature recommends the association of the pelvis in spine instrumentation as gold standard in the surgical management of patients with neuromuscular scoliosis associated with pelvic obliquity (6,7). This can be achieved by performing solid instrumentations of the spine, including the pelvis, with fusions that allow good balance in the sagittal and coronal planes (8).
Different surgical techniques for fixation of the pelvis have been developed. One of the first techniques for the management of patients with neuromuscular scoliosis is the Galveston technique, developed by Allen and Ferguson (9) in 1980, which comprises the placement of fixing bars to the ilium. Later, Luque popularized the use of sublaminar wires for segmental fixation, which have been widely combined with the Galveston technique (10,11).
Other techniques include the use of S-shaped molded bars on the sacral ala, known as the Dunn McCarthy technique, evolving into the placement of iliac screws and finally, to the fixation with S2 alar iliac (S2AI) screws. The latter has demonstrated an improvement in the correction of the deformity, lower rates of pseudoarthrosis and a decrease in the requirement of anterior approaches (12,13) but still the current information is not conclusive.
In our hospital, these different techniques for the management of neuromuscular scoliosis have evolved over time. For several years, we have implemented the technique described by Sponseller et al. (13). Therefore, we decided to conduct this study in order to evaluate the radiological outcomes and secondary adverse events associated with this surgical technique in our population.
Methods
An observational case series study was performed. The hospital spinal surgery database was reviewed between January 2011 and February 2014 and all pediatric patients diagnosed with neuromuscular scoliosis associated with pelvic obliquity, which required surgery with fixation unto S2AI, were included.
Variables assessed in this study were: sociodemographic characteristics, radiographic pelvic obliquity, those related to the surgical procedure and adverse events during surgery. Patients with concomitant congenital spinal malformations, incomplete medical records and those without radiographic images available, were excluded.
The surgical technique used for placement of the S2AI screws was the one described by Sponseller et al. (13), in which the reference for the screw placement is a midpoint between the foramina of S1 and S2, angled 40° laterally and 40° caudally. Preoperative and postoperative radiographic assessment of the spino-pelvic angle of all patients was performed in the anterior-posterior projection by the method proposed by Maloney (14), estimating the pelvic obliquity by measuring the angle between a line from the middle of T1 to the middle of S1 and a line perpendicular to the latter from one iliac crest to the contralateral.
Statistical analysis
Demographic characteristics of patients are presented in descriptive tables. Clinical and radiological findings, and adverse events are presented with measures of central tendency. Comparison of deformity correction was carried out using a non-parametric analysis for related samples (Wilcoxon signed-rank test).
The effect size was rated according to the Cohen’s guide: small =0.2 to 0.5; medium =0.5 to 0.8; and large = greater than 0.8 (15). The results were analyzed with the statistical software IBM SPSS Statistics® version 21.
Results
A total of 31 patients diagnosed with neuromuscular scoliosis that met inclusion criteria were analyzed. From these, 54.8% of patients were females. Mean age at time of surgery was 14.39±6.77 years. The leading cause of neuromuscular scoliosis in 23 (74.2%) patients was spastic CP. The remaining sociodemographic characteristics are described in Table 1.
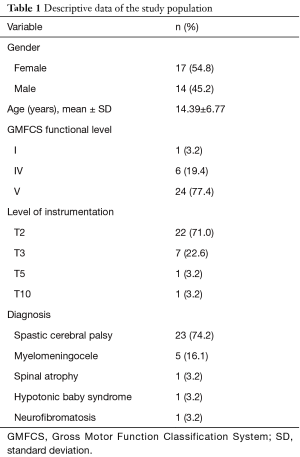
Full table
Table 2 summarizes the surgical variables comparing the first with the second surgical stage. Intraoperative bleeding was higher in the second surgical stage compared to the first stage (1,528.5±784.6 vs. 1,367.7±1,001.7).
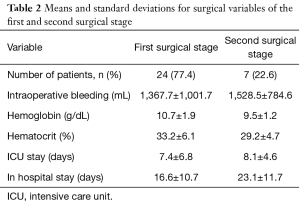
Full table
Mean follow-up time was 9±7 months. In this sample of patients, it was found that the correction of pelvic obliquity in the immediate postoperative period was of 76%, which is statistically significant. The effect size was 1.35, and was interpreted as large. In addition, the extent of correction that patients maintained at the end of the follow-up was analyzed, and it was found that there were no significant differences in this magnitude, compared with the immediate postoperative pelvic obliquity (Table 3).
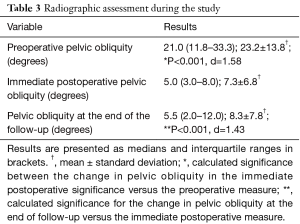
Full table
Adverse events occurred in 64.5% of patients. Intraoperative events were: pleural injury in the 1.9% of these patients and poor positioning of screws in 1.9%. The last one is a patient that presented with an intra-articular screw in the left hip that required repositioning. Regarding postoperative adverse events, it was found that infections were the most common outcome: pneumonia occurred in 14.8% of patients, followed by surgical site infection in 7.4%.
A rate of 12.9% of pulmonary events was found, mainly due to respiratory failure, hemo-pneumothorax, pleural effusion and atelectasis. The remaining intraoperative and postoperative adverse events are described in Table 4.
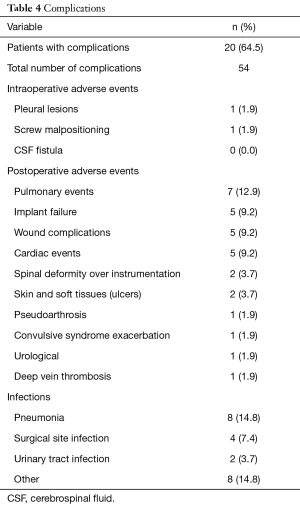
Full table
Discussion
Pelvic fixation in the surgical management of neuromuscular scoliosis remains a major challenge as well as a point of controversy. Over time, fixation methods have evolved from early configurations of the Galveston technique, to the S2AI screws placement described by Sponseller et al. in 2009, a technique that has been adopted in our practice since 2010 for management of pelvic obliquity (9-11,13).
Different studies have evidenced the advantages of the S2AI screw technique, among which a better correction of the deformity and preservation during the follow-up, lower rate of pseudoarthrosis, less soft tissue injuries associated with the prominence of instrumentation and lower rate wound complications can be found (16-18).
There are some biomechanical advantages with the use of this technique, including a lower rate of screw pull-out (9). In the study of Sutterlin et al. (19), a biomechanical comparison between S2AI screws with traditional fixation strategies was made, he concluded that from a biomechanical standpoint S2AI technique is equivalent to traditional iliac screws but offers some extra benefits like, lower profile instrumentation, easier alignment with cephalad fixation, and ease of assembly without the need for lateral connectors which also reduces costs.
In our series, surgery for the correction of scoliosis extended down to S2AI was more common in females, in opposition to what has been reported by Shabtai et al. (20) and other publications (17,21).
CP remains to be the main cause of neuromuscular scoliosis present in 74.2% of cases, followed by myelomeningocele in a 16.1%, consistent with the study by Funk et al. (16).
The extent of neurological involvement influences the decision-making process regarding the level of instrumentation both proximally and distally; we found that 71% of patients required instrumentation beginning in T2, followed by T3 in 22.6%, similar to what Schoenleber et al. (17) reported, in which 77.3% of fixations started in T2 and 15.9% in T3.
Considering the amount of surgical exposure required in these patients to correct scoliosis, usually ranging from the first thoracic vertebrae to sacral, surgical bleeding is high. Bleeding in the first surgical stage was 1,367±1,001 and 784±1,528 mL in the second, lower than the one reported by Moon et al. (21), which reported an intraoperative bleeding of 2,700 mL in the surgical management of pelvic obliquity in patients with neuromuscular scoliosis.
The percentage of correction of pelvic obliquity in our patients was 76%: the pelvic tilt angle went from 21° (11.8°–33.3°) preoperatively to a postoperative angle of 5° (3°–8°) and at the end of the follow-up this correction was maintained at 5.5° (2°–12°) without statistical significance between the last two measurements. Schoenleber et al. (17), reported an average preoperative pelvic obliquity of 29.9°±12.8° with a postoperative correction at 2 years of 5.3°±4.9°, representing a rate of correction of 77%, very similar to what was found in our results.
In the surgical treatment of neuromuscular scoliosis, the rate of adverse events in different publications ranges between 44% and 80%, with mortality rates from 0 to 7% (22). A total of 64.5% of adverse events were presented in this study. These events were divided into intraoperative, postoperative complications and infections.
Among intraoperative adverse events found in this series, intraoperative pleural injury and screw malpositioning were found in 1.9% of the cases. This rate is lower than the one reported in the meta-analysis by Sharma et al. (23), in which a rate of complications of 4.81% was found. This case of screw malpositioning occurred in a patient with CP, in which the implantation of a longer screw invaded the left hip and required revision surgery in order to change the screw for a shorter one.
The most common postoperative complications were those of respiratory origin found in 18.4% of patients. This rate is similar to what has been found by other authors that describe rates of respiratory complications up to 22.7% (23). Respiratory failure, hemo-pneumothorax, pleural effusion and atelectasis were the main manifestations of these respiratory events related to neuromuscular scoliosis (24).
In a comparative study between fixation to the ilium wings versus fixation with S2AI screws for the management of neuromuscular scoliosis by Shabtai et al. (20), implant failure was found in 24% for the first group versus 7% for the second. In our study implant failure was documented in 9.2% of patients, which was slightly higher than the rate reported by this author.
The rate of events related with surgical wounds was 13.2%, which include the presence of seroma and wound dehiscence. Additionally, prominence of implants was found in 3.7% of patients, a much lower rate than the one reported by Funk et al. (16), who found a wound complication rate of 10.5%.
The stiffness of implants for the management of neuromuscular scoliosis has evolved in order to improve consolidation rates and prevent non-union. Different series have reported a decrease in the rates of failure depending on the technique used. With the Luque-Galveston technique, the rate of this complication ranges between 7% to 17%, and with the S2AI screws technique this rate is up to 10.5% (16). In our study, the rate of pseudoarthrosis was 1.9%, lower than the aforementioned rates.
Infection remains as one of the main concerns in patients with neuromuscular diseases, as their higher number of comorbidities makes them more susceptible to this complication. The rate of superficial and deep surgical site infections after fixation to the pelvis in the management of neuromuscular scoliosis is estimated to be between 4.2% and 20% (18,21,25,26), range in which our results fall, showing a rate of surgical site infection of 7.4%.
Pneumonia as a postoperative complication was present in 14.8%, higher than the reported by Rawlins et al. (27), who described that this complication occurs in 1 of every 15 patients with neuromuscular scoliosis.
Non-ambulatory patients with neuromuscular diseases might have an increased risk of adverse events with an OR 3.2 (95% CI: −7.4 to 1.4) (P<0.01) (24). Since all of our patients were non-ambulatory and 77.4% had a GMFCS functional level of V, this could explain our results, where an overall rate of adverse events of 64.5% was found.
The limitations of this study are those characteristics of a retrospective study. X-rays are not obtained with a standardized technique. In addition, there is no control group of patients in order to establish associations between the surgical procedure and its favorable or unfavorable outcomes.
S2AI fixation for the treatment of neuromuscular scoliosis is a safe alternative, in which the onset of complications is related to the comorbidities of patients instead of the surgical procedure itself. An approximate correction of 76% is maintained during the follow-up, assisting the management of these patients to their caregivers.
Acknowledgements
The authors thank Dr. Daniel Uruchi for gathering patient information, and Dr. Ricardo Mendez for his advice with the results section.
Footnote
Conflicts of Interest: This study was submitted as an abstract for a medical meeting.
Ethical Statement: In accordance with the Colombian resolution number 008430/1993 and in conform with the provisions of the declaration of Helsinki the protocol for the present study was approved by the ethics committee of the institution.
References
- Saito N, Ebara S, Ohotsuka K, et al. Natural history of scoliosis in spastic cerebral palsy. Lancet 1998;351:1687-92. [Crossref] [PubMed]
- Hodgkinson I, Bérard C, Chotel F, et al. Pelvic obliquity and scoliosis in non-ambulatory patients with cerebral palsy: a descriptive study of 234 patients over 15 years of age. Rev Chir Orthop Reparatrice Appar Mot 2002;88:337-41. [PubMed]
- Thometz JG, Simon SR. Progression of scoliosis after skeletal maturity in institutionalized adults who have cerebral palsy. J Bone Joint Surg Am 1988;70:1290-6. [Crossref] [PubMed]
- Olafsson Y, Saraste H, Al-Dabbagh Z. Brace treatment in neuromuscular spine deformity. J Pediatr Orthop 1999;19:376-9. [Crossref] [PubMed]
- Peelle MW, Lenke LG, Bridwell KH, et al. Comparison of pelvic fixation techniques in neuromuscular spinal deformity correction: Galveston rod versus iliac and lumbosacral screws. Spine (Phila Pa 1976) 2006;31:2392-8. [Crossref] [PubMed]
- Neustadt JB, Shufflebarger HL, Cammisa FP. Spinal fusions to the pelvis augmented by Cotrel-Dubousset instrumentation for neuromuscular scoliosis. J Pediatr Orthop 1992;12:465-9. [Crossref] [PubMed]
- Arlet V, Marchesi D, Papin P, et al. The “MW”sacropelvic construct: an enhanced fixation of the lumbosacral junction in neuromuscular pelvic obliquity. Eur Spine J 1999;8:229-31. [Crossref] [PubMed]
- Obid P, Bevot A, Goll A, et al. Quality of life after surgery for neuromuscular scoliosis. Orthop Rev (Pavia) 2013;5:e1. [Crossref] [PubMed]
- Allen BL Jr, Ferguson RL. The Galveston technique of pelvic fixation with L-Rod instrumentation of the spine. Spine (Phila Pa 1976) 1984;9:388-94. [Crossref] [PubMed]
- Luque ER. The anatomic basis and development of segmental spinal instrumentation. Spine (Phila Pa 1976) 1982;7:256-9. [Crossref] [PubMed]
- Luque ER. Segmental spinal instrumentation for correction of scoliosis. Clin Orthop Relat Res 1982.192-8. [PubMed]
- McCarthy RE, Bruffett WL, Mc-Cullough FL. S rod fixation to the sacrumin patients with neuromuscular spinal deformities. Clin Orthop Relat Res 1999.26-31. [Crossref] [PubMed]
- Sponseller PD, Zimmerman RM, Ko PS, et al. Low profile pelvic fixation with the sacral alar iliac technique in the pediatric population improves results at two-year minimum follow-up. Spine (Phila Pa 1976) 2010;35:1887-92. [Crossref] [PubMed]
- Maloney WJ, Rinsky LA, Gamble JG. Simultaneous correction of pelvic obliquity, frontal plane, and sagittal plane deformities in neuromuscular scoliosis using a unit rod with segmental sublaminar wires: a preliminary report. J Pediatr Orthop 1990;10:742-9. [Crossref] [PubMed]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd edn. Hillsdale, New Jersey: L. Erlbaum, 1988.
- Funk S, Lovejoy SA, Mencio GA, et al. Rigid Instrumentation for Neuromuscular Scoliosis Improves Deformity Correction Without Increasing Complications. Spine (Phila Pa 1976) 2016;41:46-52. [Crossref] [PubMed]
- Schoenleber SJ, Asghar J, Bastrom TP, et al. Are S1 Screws a Useful Adjunct to Iliac Screws in Long Fusions to the Sacrum in Cerebral Palsy? Spine (Phila Pa 1976) 2016;41:139-45. [Crossref] [PubMed]
- Sponseller PD, LaPorte DM, Hungerford MW, et al. Deep wound infections after neuromuscular scoliosis surgery: a multicenter study of risk factors and treatment outcomes. Spine (Phila Pa 1976) 2000;25:2461-6. [Crossref] [PubMed]
- Sutterlin CE 3rd, Field A, Ferrara LA, et al. Range of motion, sacral screw and rod strain in long posterior spinal constructs: a biomechanical comparison between S2 alar iliac screws with traditional xation strategies. J Spine Surg 2016;2:266-76. [Crossref] [PubMed]
- Shabtai L, Andras LM, Portman M, et al. Sacral Alar Iliac (SAI) Screws Fail 75% Less Frequently Than Iliac Bolts in Neuromuscular Scoliosis. J Pediatr Orthop 2017;37:e470-e475. [Crossref] [PubMed]
- Moon ES, Nanda A, Park JO, et al. Pelvic Obliquity in Neuromuscular Scoliosis Radiologic Comparative Results of Single-Stage Posterior Versus Two-Stage Anterior and Posterior Approach. Spine (Phila Pa 1976) 2011;36:146-52. [Crossref] [PubMed]
- Broom MJ, Banta JV, Renshaw TS. Spinal fusion augmented by Luque-rod segmental instrumentation for neuromuscular scoliosis. J Bone Joint Surg Am 1989;71:32-44. [Crossref] [PubMed]
- Sharma S, Wu C, Andersen T, et al. W Prevalence of complications in neuromuscular scoliosis surgery: a literature meta-analysis from the past 15 years. Eur Spine J 2013;22:1230-49. [Crossref] [PubMed]
- Master DL, Son-Hing JP, Poe-Kochert C, et al. Risk Factors for Major Complications After Surgery for Neuromuscular Scoliosis. Spine (Phila Pa 1976) 2011;36:564-71. [Crossref] [PubMed]
- Ramo BA, Roberts DW, Tuason D, et al. Surgical site infections after posterior spinal fusion for neuromuscular scoliosis: a thirty year experience at a single institution. J Bone Joint Surg Am 2014;96:2038-48. [Crossref] [PubMed]
- Reames DL, Smith JS, Fu KM, et al. Complications in the Surgical Treatment of 19,360 Cases of Pediatric Scoliosis. Spine (Phila Pa 1976) 2011;36:1484-91. [Crossref] [PubMed]
- Rawlins BA, Winter RB, Lonstein JE, et al. Reconstructive spine surgery in pediatric patients with major loss in vital capacity. J Pediatr Orthop 1996;16:284-92. [Crossref] [PubMed]


