Influence of psychosocial distress in the results of elective lumbar spine surgery
Introduction
Diverse pathological entities are known to cause low back pain and more recently, literature have testified the role of environmental and psychosocial factors in the presentation of spinal related symptoms. The large number of patients complaining about lumbar pain and its consequent social and financial impact are alarming the medical organizations to consider psychosocial components that may influence or attenuate the clinical presentation. Among the factors known to influence clinical presentation are as psychological conditions, litigation, social and work status, and other secondary gains (1,2).
Back pain has been associated with mental health comorbidities, such as depressive episodes, psychosis diagnosis, anxiety, sleep disturbance and high levels of stress (3). Although, low back pain not only correlated with mental and behavior status, but can affect the labor ability, creating both financial and emotional issues (4). Literature have shown that psychosocial factors are able to negatively influence the clinical presentation and the outcomes of spine surgery (1,5-11).
Presurgical screening have been successful in establishing the relationship between particular psychological (12-16) and social (4,10,17-19) issues with clinical outcomes and patient satisfaction. Different risk factors were identified to independently impact surgical outcomes: work compensation (10,17,18,20), lifestyle factors (21), expectations (22-24), depression (13,16,25), anxiety (26), substance use and abuse (27,28), and preoperative education (29,30). However, the appreciation of the patient’s psychological distress is used as a routine by few spine services (31).
Epker and Block (32) have suggested that if two or more of the following criteria are met, the surgeon must consider the case for presurgical psychological screening: inconsistent symptoms; high levels of depression or anxiety; sleep disturbance; excessively high or unrealistically low expectations; marital distress or sexual difficulties; emotional lability or mood swings; not working or decreased function greater than 2 months; large or escalating doses of narcotics or anxiolytics; worker’s compensation or pending litigation; history of non-compliance with medical treatment; history of psychiatric or psychological treatment, or suspected major psychopathology. In the surgeon’s daily routine, it may be demanding to consider all criteria, and even if it is done, spinal surgeons can fail to detect all these distresses (33). The efforts on developing a presurgical screening aim to identify the psychosocial risk in a comprehensive and independent way (31,34,35).
The objective of this study was to analyze the surgical outcomes following systematic and independent presurgical screening in patients undergoing elective lumbar fusion.
Methods
Prospective collected data was retrospective collected [2011–2016] from a non-randomized cohort at a single center. Inclusion criteria: elective lumbar interbody fusion for lumbar lumbosciatalgia due to degenerative conditions from 1 up to 3 spine levels; psychological evaluation at the same spine center before surgery; minimum 6-month follow-up. Exclusion criteria: cases with severe psychosocial issues found during the psychosocial evaluation; incomplete medical chart.
Routinely in our spine center, all patients with medical indication to an instrumented lumbar interbody fusion undergo to a presurgical psychosocial screening. A psychologist performed the evaluation with a semi-structured interview following the same steps for every patient. The parameters collected were: depression (HAD-D questionnaire) (36,37), anxiety (HAD-A questionnaire) (36,37), previous psychological/psychiatric treatment, abuse of prescription or illegal drugs, alcohol usage, sleep quality, marital status, employment status, litigation, any compensation with the condition (whether marital, social, financial), diagnosis and treatment understanding, suitability of coping strategies, and suitability of expectations.
Despite subjective, the following parameters were considered as yellow flags: previous spine surgery, worker’s compensation, illicit drugs usage, previous psychiatric treatment, any compensation regarding the condition, not suitable diagnosis and treatment understanding, suitable expectancies, anxiety, and depression. Every item from the interview was included into a database for further analysis. Resulting from this evaluation, the psychologist concludes with one of three possible status: mild psychosocial issues (supportive to surgery); moderate psychosocial issues (supportive to surgery with reservation); severe psychosocial issues (not supportive to surgery). For this work, the cases were divided into two groups: mild psychosocial issues (green group) and moderate psychosocial issues (yellow group). Patients with severe psychosocial issues usually does not follow immediately for surgery, so they were not included in the present work.
In addition to the psychosocial variables, demographic and pathology information were analyzed in this study as well. The following scales were used as clinical endpoints: visual analogue scale (VAS) (to assess pain levels), Oswestry disability index (38) (ODI) (to assess physical disability), and EuroQol 5D (39) (EQ-5D) (to assess quality of life) at the preoperative visit and at postop follow-up (6–12 months after surgery).
Descriptive and comparative analyzes were applied. Minimal clinically important difference (MCID) method was used according to previous published data in order to access clinical relevance in pain scores [minimum, 1.2 points in VAS (40)], disability [minimum, 12.8 points in ODI (40)] and quality of life [minimum, 0.08 points in EQ-5D (41)]. Statistical analyses were performed with Student’s t-test, Fisher’s exact test, and one-way ANOVA with an alpha of 0.05.
Results
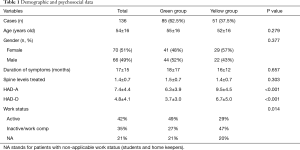
A total of 196 patients were first selected and 58 were excluded due to missing data. Two patients (2/138, 1.4%) were excluded due severe psychosocial issues and 136 were included in the analysis. A total of 195 spine levels were fused (average, 1.4 levels per case), and all surgeries were lumbar interbody fusions, either by the posterior, lateral or anterior approach. Demographic data is shown in Table 1. Mean age was 54 (range, 19–89) years old and 51% (70/136) were female. The enrollment by groups presented as follows: 85 cases in the green group (62.5%) and 51 in the yellow group (37.5%). Demographic and psychological data divided per group is provided in Table 1. The groups (green and yellow, respectively) had similar values in the following parameters: mean age (55 vs. 52 years old; P=0.279); spine levels treated (1.5 vs. 1.4; P=0.303); duration of the symptoms (18.0 vs. 16.0 months; P=0.657). The division of the study cohort into mild and moderate was confirmed with the difference seen in the HAD-D and HAD-A scales, 3.7 vs. 6.7 (P<0.001) and 6.3 vs. 9.5 (P<0.001), respectively for the green and yellow group. Despite the subjective characteristic of the preoperative psychosocial evaluation, it was possible to observe that the allocation into green and yellow groups resulted from an objective criterion: patients allocated into the yellow group had more yellow flags compared to green group (average: 2.5; SD, 1.5; 95% CI: 2.1–2.9 vs. 1.2; SD, 1.1; 95% CI: 1.0–1.4).
Full table
Pre-operative and follow-up clinical outcomes are shown in Figures 1-3. While it was observed that both groups presented similar VAS values at the preoperative visit (5.9 vs. 6.3; green and yellow, respectively; P=0.163), the green group evolved with lower pain levels after surgery (2.7 vs. 3.7; P=0.003; Figure 1). The improvement in VAS scores was 54% and 41%, respectively, but not significantly different between groups (P=0.443). In the ODI scale, the green group already presented lower values preoperatively compared to yellow cohort (44 vs. 51; P=0.009), and remained with lower levels after surgery (25 vs. 33; P=0.049; Figure 2). The improvement in ODI scores was 43% and 35%, respectively, but not significantly different between groups (P=0.740). In EQ-5D scale the green group had better scores compared to yellow cohort before surgery (0.59 vs. 0.47; P=0.03) and at the postoperative assessment (0.74 vs. 0.64; P=0.017; Figure 3). The improvement in EQ-5D scale was 20% and 27%, respectively, but not significantly different among the groups (P=0.796).
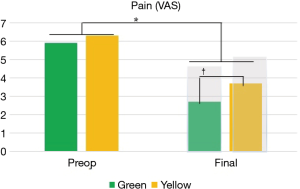
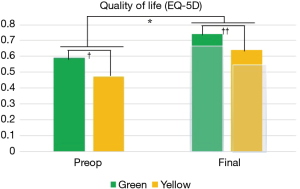
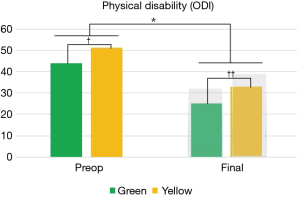
Despite the yellow group have shown poorer postoperative clinical outcomes compared to the green group, both groups demonstrated clinical improvements superior to MCID in the three different clinical self-assessed questionnaires. The MCID values for each domain are represented by the shaded bars in Figures 1-3.
Additionally, it was searched the impact of particular psychosocial parameters into the final outcomes. It was possible to testify that work compensation had a negative impact in clinical outcomes: VAS 4.9 vs. 3.2 (P=0.021; F=5.575), ODI 34.7 vs. 23.3 (P=0.011; F=6.730), EQ-5D 0.59 vs. 0.75 (P=0.002; F=10.812), respectively for subject with and without work compensation. Depression demonstrated relation with poorer results in ODI (P=0.036; F=3.468) and EQ-5D (P=0.002; F=6.677), in contrast to the presence of anxiety, which was not significantly related to altered outcomes. Other three parameters analyzed were related to poorer clinical outcomes: not suitable comprehension of the diagnosis and/or treatment (ODI: P=0.005, F=5.620; EQ-5D: P<0.001, F=12.335); presence of social/familiar/financial compensation due to pathology (VAS: P=0.012, F=5.078; ODI: P=0.001, F=8.694; EQ-5D: P=0.014, F=4.781); previous spine surgery (VAS: P=0.001, F=11.547; ODI: P<0.001, F=15.580; EQ-5D: P<0.001, F=14.594). The following parameters were not related to final clinical outcomes: gender, alcohol usage, illicit drugs usage, previous psychological treatments, previous psychiatric treatments, suitable coping strategies, sexual life status, quality of sleep, and suitable expectancies.
Discussion
In this study, all patients undergoing elective lumbar fusion were referred to presurgical psychological screening. As result of the screening, patients were divided in mild psychosocial issues (green group), moderate psychosocial issues (yellow group) or severe psychosocial issues (surgeon reconsidered surgery). Patients in the yellow group, with moderate psychosocial issues, have higher level of depression, secondary gains and/or work compensation and evolve with worse results following elective lumbar spine surgery. The results from this study revealed that patients presenting significant psychosocial distress at the time of surgical indication had lower quality of life and more severe physical disability.
It is well known that some psychopathologies might distort the perception of pain and disability, and then may increase the dysfunction related to the painful illness (2,5). Patients with psychiatric disorders often complain about chronic pain, not rarely in various segments of the body in the absence of a pathological finding (42). Low back pain is highly associated with mental health comorbidities: stress sensitivity, poor pain copying, anxiety, psychosis spectrum, and especially with depression conditions (3,7). A number of studies have found an association between psychological factors and spine surgery results, and depression has been the most reported factor, although anxiety, stress, distress, mood, and poor cognitive functioning have also been associated with inferior results (8,13,16,25,26,43).
The hospital anxiety and depression (HAD) scale has been developed and found to be a reliable instrument for detecting states of depression and anxiety in the setting of a hospital medical outpatient clinic rather than psychiatric sample (37). The HAD scale has advantages over other assessments of anxiety and depression; it is efficient in assessing both anxiety and depression with a total of 14 items. This scale has been validated and used in spine clinical studies around the world (7,15,44-46). Other popular instrument used to assess psychological alterations is the Distress and Risk Assessment Method (DRAM) (47), a combination of the Zung Depression Scale and the Modified Somatic Perception Questionnaire.
Not only psychological distress, but also lifestyle and social issues are more prevalent in individuals with LBP (2,48-50) and represent an additional challenge for the treatment. Substance use and abuse, conflictual interpersonal relationships, marital status, workplace factors, litigation, and workers’ compensation represents problems that can aggravate clinical presentation and results following the treatment (10,17-19,51). The most relevant social parameter in relation to spine surgery according to the recent literature and corroborated by our study is the presence of workers’ compensation. Patients receiving workers’ compensation tend to have inferior outcomes after spine surgery. In a meta-analysis of 31 studies, Cheriyan et al. (1) testified that workers’ compensation patients have a two-fold increased risk of an unsatisfactory outcome. In addition, some cumulative risk factors over workers’ compensation were identified, such as prolonged opioid use, legal representation, and finally, depression as the stronger predictor of poor lumbar fusion outcomes among workers’ compensation subjects (13,52,53).
Psychological, social, labor and clinical issues are in an intimate and complex relationship within a person. Picking just one parameter from this pack, whether psychological or social, might represent an incomplete picture of the whole problem. For this reason, a complete psychosocial analysis should be performed by adopting different and validated tools. Despite the helpful support of these tools, they do not substitute the nature of a face-to-face psychological interview. Separately, as one isolate entity, the occurrence of either anxiety disorder, depression or work compensation may not be decisive itself, but the combination of some these yellow flags can endorse the diagnose of an unfavorable presentation.
There is solid evidence that providing information, adequate support services, discussion of expectations, and multidisciplinary programs significantly improve the quality of life and then proportionate superior results (54-56). Daubs and colleagues (33) found that spinal surgeons have low sensitivity rates to detect this distress, and the use of simple clinical impression should be give place to standardized methods of analysis. It has been highly recommended a preoperative psychosocial evaluation of the cases elected to spine surgery through a professional, independent, multidisciplinary and comprehensive way (34). Not every mild psychological or social disturbance will guarantee a poor outcome (57), but using a presurgical assessment both the surgeon and the patient can be aware of a certain predisposition that can contribute with poorer surgical results. It is not clear how cognitive-behavioral interventions could improve results following surgery, although some study groups (58-61) have found beneficial effect of combined rehabilitation strategies. This is a field that deserves further research.
Some limitations of the current study must be pointed out. The limited number of patients included is a major issue, and the expansion of this number is needed for a more powerful multivariate analysis in order to stablish the particular role of each of the psychosocial parameters. The second limitation is the retrospective study design itself, although the data had been collected prospectively along the years. A third limitation lays in the single-center experience. Finally and most important, the psychological evaluation before the surgeries was performed using the basis of the psychological science: interpretation done by a psychologist, and therefore it is an subjective process. In order to diminish the subjectivity of this evaluation, this and other groups (34) have used semi-structured interview with the same steps for psychometric testing and validated scales for each and every patient.
Conclusions
Psychosocial factors are related to different degrees of clinical impairment and quality of life in the preoperative period and they can influence the final surgical result. A preoperative psychological evaluation may identify in a simplified way to the surgeon the presence of psychosocial distress related with poorer results. Overall, this study demonstrated that spine surgery, even in patients with moderate psychosocial risk, is effective in providing significant relief of pain, improvements in functional ability and quality of life. However, both the patient and the surgeon must be aware that presence of moderate psychosocial distress may affect clinical presentation and surgical results.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by Hospital Nove de Julho (No. 2.230.365) and written informed consent was obtained from all patients.
References
- Cheriyan T, Harris B, Cheriyan J, et al. Association between compensation status and outcomes in spine surgery: a meta-analysis of 31 studies. Spine J 2015;15:2564-73. [Crossref] [PubMed]
- Moore JE. Chronic low back pain and psychosocial issues. Phys Med Rehabil Clin N Am 2010;21:801-15. [Crossref] [PubMed]
- Stubbs B, Koyanagi A, Thompson T, et al. The epidemiology of back pain and its relationship with depression, psychosis, anxiety, sleep disturbances, and stress sensitivity: Data from 43 low- and middle-income countries. Gen Hosp Psychiatry 2016;43:63-70. [Crossref] [PubMed]
- Mathew J, Singh SB, Garis S, et al. Backing up the stories: The psychological and social costs of chronic low-back pain. Int J Spine Surg 2013;7:e29-38. [Crossref] [PubMed]
- Teixiera MJ. Chronic pain and depression. Rev Neurocienc 2006;14:44-53.
- Falavigna A, Righesso Neto O, Teles AR. Avaliação clínica e funcional no pré-operatório de doenças degenerativas da coluna vertebral. Coluna/Columna 2009;8:245-53. [Crossref]
- Amaral V, Marchi L, Oliveira L, et al. Prevalence and relationship of emotional and clinical factors in patients with degenerative disc disease. Coluna/Columna 2010;9:150-6. [Crossref]
- Trief PM, Grant W, Fredrickson B. A prospective study of psychological predictors of lumbar surgery outcome. Spine 2000;25:2616-21. [Crossref] [PubMed]
- Adogwa O, Carr K, Fatemi P, et al. Psychosocial factors and surgical outcomes: are elderly depressed patients less satisfied with surgery? Spine 2014;39:1614-9. [Crossref] [PubMed]
- Motter BV, Machado AN, Brandão TK, et al. Quality of Life in Patients Before and After Lumbar Surgery in Different Work Situations. Coluna/Columna 2015;14:198-201. [Crossref]
- Adogwa O, Elsamadicy AA, Cheng J, et al. Independent predictors of reliability between full time employee-dependent acquisition of functional outcomes compared to non-full time employee-dependent methodologies: a prospective single institutional study. J Spine Surg 2016;2:47-51. [Crossref] [PubMed]
- Abtahi AM, Brodke DS, Lawrence BD, et al. Association Between Patient-Reported Measures of Psychological Distress and Patient Satisfaction Scores in a Spine Surgery Patient Population. J Bone Joint Surg Am 2015;97:824-8. [Crossref] [PubMed]
- Anderson JT, Haas AR, Percy R, et al. Clinical depression is a strong predictor of poor lumbar fusion outcomes among workers’ compensation subjects. Spine 2015;40:748-56. [Crossref] [PubMed]
- Consciência JA de CG. Psychosomatic and clinical progression of patients with stenosis of lumbar canal undergoing surgery with interspinous system. Coluna/Columna 2013;12:212-7.
- Skeppholm M, Fransson R, Hammar M, et al. The association between preoperative mental distress and patient reported outcome measures in patients treated surgically for cervical radiculopathy. Spine J 2017;17:790-8. [Crossref] [PubMed]
- Theologis AA, Ailon T, Scheer JK, et al. Impact of preoperative depression on 2-year clinical outcomes following adult spinal deformity surgery: the importance of risk stratification based on type of psychological distress. J Neurosurg Spine 2016;25:477-85. [Crossref] [PubMed]
- Anderson PA, Schwaegler PE, Cizek D, et al. Work status as a predictor of surgical outcome of discogenic low back pain. Spine 2006;31:2510-5. [Crossref] [PubMed]
- Haddad GH. Analysis of 2932 workers’ compensation back injury cases. The impact on the cost to the system. Spine 1987;12:765-9. [Crossref] [PubMed]
- Vereckei E, Susanszky E, Kopp M, et al. Psychosocial, educational, and somatic factors in chronic nonspecific low back pain. Rheumatol Int 2013;33:587-92. [Crossref] [PubMed]
- Mobbs RJ, Gollapudi PR, Chandran NK. Outcome following anterior cervical discectomy in compensation patients. J Clin Neurosci 2001;8:124-5. [Crossref] [PubMed]
- Schwartz CE, Quaranto B, Samaha E, et al. Relevance of Lifestyle and Attitudinal Factors to Spine Surgery Outcomes: Empirical Results on a Heterogeneous Sample. Surg Sci 2011;2:121. [Crossref]
- Carr FA, Healy KM, Villavicencio AT, et al. Effect on clinical outcomes of patient pain expectancies and preoperative Mental Component Summary scores from the 36-Item Short Form Health Survey following anterior cervical discectomy and fusion. J Neurosurg Spine 2011;15:486-90. [Crossref] [PubMed]
- Iversen MD, Daltroy LH, Fossel AH, et al. The prognostic importance of patient pre-operative expectations of surgery for lumbar spinal stenosis. Patient Educ Couns 1998;34:169-78. [Crossref] [PubMed]
- Myers SS, Phillips RS, Davis RB, et al. Patient expectations as predictors of outcome in patients with acute low back pain. J Gen Intern Med 2008;23:148-53. [Crossref] [PubMed]
- Adogwa O, Parker SL, Shau DN, et al. Preoperative Zung Depression Scale predicts outcome after revision lumbar surgery for adjacent segment disease, recurrent stenosis, and pseudarthrosis. Spine J 2012;12:179-85. [Crossref] [PubMed]
- Li S, Qi M, Yuan W, et al. The impact of the depression and anxiety on prognosis of cervical total disc replacement. Spine 2015;40:E266-71. [Crossref] [PubMed]
- Lee D, Armaghani S, Archer KR, et al. Preoperative Opioid Use as a Predictor of Adverse Postoperative Self-Reported Outcomes in Patients Undergoing Spine Surgery. J Bone Joint Surg Am 2014;96:e89. [Crossref] [PubMed]
- Spengler DM, Freeman C, Westbrook R, et al. Low-back pain following multiple lumbar spine procedures. Failure of initial selection? Spine 1980;5:356-60. [Crossref] [PubMed]
- Papanastassiou I, Anderson R, Barber N, et al. Effects of preoperative education on spinal surgery patients. SAS J 2011;5:120-4. [Crossref] [PubMed]
- Devine EC. Effects of psychoeducational care for adult surgical patients: a meta-analysis of 191 studies. Patient Educ Couns 1992;19:129-42. [Crossref] [PubMed]
- Young AK, Young BK, Riley LH, et al. Assessment of presurgical psychological screening in patients undergoing spine surgery: use and clinical impact. J Spinal Disord Tech 2014;27:76-9. [Crossref] [PubMed]
- Epker J, Block AR. Psychological Screening Before Spine Surgery: Avoiding Failed Surgery Syndrome. Psychol Inj Law 2014;7:317-24. [Crossref]
- Daubs MD, Patel AA, Willick SE, et al. Clinical impression versus standardized questionnaire: the spinal surgeon’s ability to assess psychological distress. J Bone Joint Surg Am 2010;92:2878-83. [Crossref] [PubMed]
- Block AR, Ohnmeiss DD, Guyer RD, et al. The use of presurgical psychological screening to predict the outcome of spine surgery. Spine J 2001;1:274-82. [Crossref] [PubMed]
- Block AR. editor. Presurgical Psychological Screening in Chronic Pain Syndromes: A Guide for the Behavioral Health Practitioner. New Jersey: Psychology Press, 1996.
- Botega NJ, Ponde MP, Medeiros P, et al. Validacao da escala hospitalar de ansiedade e depressao (HAD) em pacientes epilepticos ambulatoriais. J Bras Psiquiatr 1998;47:285-9.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70. [Crossref] [PubMed]
- Vigatto R, Alexandre NM, Correa Filho HR. Development of a Brazilian Portuguese version of the Oswestry Disability Index: cross-cultural adaptation, reliability, and validity. Spine 2007;32:481-6. [Crossref] [PubMed]
- Menezes RM, Andrade MV, Noronha KV, et al. EQ-5D-3L as a health measure of Brazilian adult population. Qual Life Res 2015;24:2761-76. [Crossref] [PubMed]
- Copay AG, Subach BR, Glassman SD, et al. Understanding the minimum clinically important difference: a review of concepts and methods. Spine J 2007;7:541-6. [Crossref] [PubMed]
- Walters SJ, Brazier JE. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res 2005;14:1523-32. [Crossref] [PubMed]
- Magni G, Caldieron C, Rigatti-Luchini S, et al. Chronic musculoskeletal pain and depressive symptoms in the general population. An analysis of the 1st National Health and Nutrition Examination Survey data. Pain 1990;43:299-307. [Crossref] [PubMed]
- Linton SJ. A review of psychological risk factors in back and neck pain. Spine 2000;25:1148-56. [Crossref] [PubMed]
- Turk DC, Dworkin RH, Trudeau JJ, et al. Validation of the Hospital Anxiety and Depression Scale in Patients With Acute Low Back Pain. J Pain 2015;16:1012-21. [Crossref] [PubMed]
- Omidi-Kashani F, Faridhoseini F, Ariamanesh S, et al. Failure Rate of Spine Surgeons in Preoperative Clinical Screening of Severe Psychological Disorders. Clin Orthop Surg 2016;8:164-7. [Crossref] [PubMed]
- Falavigna A, Righesso O, Teles AR, et al. Depression Subscale of the Hospital Anxiety and Depression Scale applied preoperatively in spinal surgery. Arq Neuropsiquiatr 2012;70:352-6. [Crossref] [PubMed]
- Main CJ, Wood PL, Hollis S, et al. The Distress and Risk Assessment Method. A simple patient classification to identify distress and evaluate the risk of poor outcome. Spine 1992;17:42-52. [Crossref] [PubMed]
- Andersson G. Epidemiology of spinal disorders. In: Frymoyer JW. editor. The adult spine: principles and practice. New York: Raven Press, 1991:107-46.
- Bigos S, Bowyer O, Braen G. Acute low back problems in adults. In: Clinical practice guideline 14. Rockville, MD, USA: Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research, 1994.
- Magnusson M, Granqvist M, Jonson R, et al. The loads on the lumbar spine during work at an assembly line. The risks for fatigue injuries of vertebral bodies. Spine 1990;15:774-9. [Crossref] [PubMed]
- Majeed SA, Vikraman CS, Mathew V, et al. Comparison of outcomes between conventional lumbar fenestration discectomy and minimally invasive lumbar discectomy: an observational study with a minimum 2-year follow-up. J Orthop Surg Res 2013;8:34. [Crossref] [PubMed]
- Anderson JT, Haas AR, Percy R, et al. Workers’ Compensation, Return to Work, and Lumbar Fusion for Spondylolisthesis. Orthopedics 2016;39:e1-8. [Crossref] [PubMed]
- DeBerard MS, LaCaille RA, Spielmans G, et al. Outcomes and presurgery correlates of lumbar discectomy in Utah Workers’ Compensation patients. Spine J 2009;9:193-203. [Crossref] [PubMed]
- Koenig TW, Clark MR. Advances in comprehensive pain management. Psychiatr Clin North Am 1996;19:589-611. [Crossref] [PubMed]
- Moradi B, Hagmann S, Zahlten-Hinguranage A, et al. Efficacy of multidisciplinary treatment for patients with chronic low back pain: a prospective clinical study in 395 patients. J Clin Rheumatol 2012;18:76-82. [Crossref] [PubMed]
- Mannion AF, Elfering A. Predictors of surgical outcome and their assessment. Eur Spine J 2006;15 Suppl 1:S93-108. [Crossref] [PubMed]
- Hobby JL, Lutchman LN, Powell JM, et al. The distress and risk assessment method (DRAM). J Bone Joint Surg Br 2001;83:19-21. [Crossref] [PubMed]
- Rolving N, Nielsen CV, Christensen FB, et al. Does a preoperative cognitive-behavioral intervention affect disability, pain behavior, pain, and return to work the first year after lumbar spinal fusion surgery? Spine 2015;40:593-600. [Crossref] [PubMed]
- Abbott AD, Tyni-Lenné R, Hedlund R. Early rehabilitation targeting cognition, behavior, and motor function after lumbar fusion: a randomized controlled trial. Spine 2010;35:848-57. [Crossref] [PubMed]
- Monticone M, Ferrante S, Teli M, et al. Management of catastrophising and kinesiophobia improves rehabilitation after fusion for lumbar spondylolisthesis and stenosis. A randomised controlled trial. Eur Spine J 2014;23:87-95. [Crossref] [PubMed]
- Christensen FB, Laurberg I, Bünger CE. Importance of the back-café concept to rehabilitation after lumbar spinal fusion: a randomized clinical study with a 2-year follow-up. Spine 2003;28:2561-9. [Crossref] [PubMed]


