Proximal junctional kyphosis in adult spinal deformity with long spinal fusion from T9/T10 to the ilium
Introduction
The goal of corrective surgery for adults with a spinal deformity is to maintain the load-bearing balance of the spine in both coronal and sagittal planes (1,2). In fact, global sagittal plane imbalance and pelvic retroversion have been associated with negative clinical outcomes after fusion (3-6). Multilevel spinal instrumented fusions are frequently necessary for the treatment of adult spinal deformity. However, with multilevel spinal fusion, high mechanical stress is concentrated on the end-points of the fusion. Consequently, it is common for proximal junctional kyphosis (PJK) to develop at the site of the upper instrumented vertebra (UIV) post-fusion. The incidence rate of PJK, after fusion, has been reported to vary between 20% and 41%, depending on the study population and the segmental range of spinal fusion (7-17). Therefore, when evaluating the risk factors for PJK, it would be important to evaluate patients having undergone the same range of fusion, as different ranges may be associated with different types of post-operative deformity. As such, the aim of our study was to evaluate the incidence rate of PJK specifically in patients having undergone long spinal fusion from the distal segments of the thoracic spine, namely T9/T10, to the ilium, and to identify risk factors for post-fusion PJK.
Identification of the risk factors for PJK is important as long spinal fusion from the distal thoracic spine to the ilium is a common surgical treatment option to manage kyphoscoliotic deformity of the thoracolumbar spine in aging adults. Risk factors were evaluated from measured radiographic variables of spinal and spinopelvic alignment. As part of our study, we were also interested in identifying the presenting clinical symptoms of PJK.
Methods
Patient selection
The study was approved by the clinical research Ethics Committee of Hamamatsu University School of Medicine and informed consent was obtained from the patients. The study group was formed of 167 adult patients, >40 years of age, who underwent posterior corrective surgery at our institution and were followed for at least 2 years after surgery. The data for the subgroup of patients who underwent fusion from T9/T10 to the ilium was extracted for analysis. All patients included in the final analysis had a complete radiographic evaluation at the three time points of assessment: pre-operatively, post-operatively, and at the end of the follow-up period.
Radiographic measurements
Radiographic assessment was performed using a standardized positioning protocol for lateral, 36-inch, standing radiographs (18). The following measures were calculated from the radiographs, at the three time points of assessment: the sagittal vertical axis (SVA), the degree of lumbar lordosis (LL) (L1–S1), the degree of thoracic kyphosis (TK) (T5–T12), pelvic tilt (PT), and the difference between the pelvic incidence and LL (PI-LL). The proximal junctional angle (PJA) was measured from the inferior endplate of the UIV to the superior endplate two levels above the UIV. An abnormal PJK was defined as a PJA >10°, with a change from pre-operative baseline >10° (19). Clinically, PJK is classified in terms of type and grade, according to the methods of Yagi et al. (20). In terms of type, PJK is classified as follows: type 1, disc and ligament failure; type 2, bone failure; and type 3, implant/bone interface failure. The grade of PJK is classified as follows: grade A, 10°–19°; grade B, 20°–29°; and grade C, ≥30°.
Clinical outcomes
The Oswestry disability index (ODI) was used to evaluate patient-reported functional outcomes, pre-operatively and 2 years after surgery.
Operative procedure
The posterior corrective surgery consisted of a standard midline approach with complete facet joint excision and use of segmental spinal pedicle screws. A Ponte osteotomy (PO), pedicle subtraction osteotomy (PSO) or vertebral column resection (VCR) was selected as the corrective technique, based on patient characteristics for each case.
Statistical analysis
Spinal alignment measures and ODI scores were presented as means and standard deviations. Differences in measured variables between patients who developed a PJK after fusion (PJK group) and those who did not develop the deformity (non-PKJ group) were evaluated using Student’s t-test for continuous variables, chi-squared analysis for dichotomous variables and Fisher’s exact test for variables with fewer than five cases. A P<0.05, with non-overlapping 95% confide intervals (CI), was considered significant. All analyses were performed using the Statistical Package for the Social Sciences (SPSS Inc., Chicago, IL, USA).
Results
Of the 167 potential patients for our study, 56 underwent corrective surgery from T9/T10 to the ilium: 7 men and 49 women, with a mean age at the time of surgery of 70.0±7.9 years (range, 41–82 years). The UIV was T9 in 19 cases and T10 in 37 cases. The following corrective techniques were used to achieve deformity correction: PO in 32 (57.1%) patients; PSO in 18 (32.1%) patients; and VCR in 6 (10.7%) patients. A PJK deformity at the final follow-up had developed in 19 of the 56 (33.9%) patients. In almost all of these 19 cases, PJK occurred within six months of surgery, with evidence of PJK observable in about 50% of these cases at the first post-operative radiographic assessment. In UIV at T9 and T10 cases, PJK occurred in 7 of the 19 (36.8%) patients and 12 of the 37 (32.4%) patients, respectively. There was no significant difference in incidence of PJK by UIV.
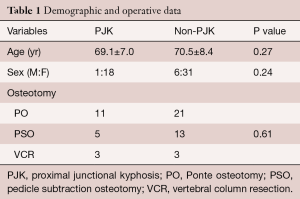
Demographic and operative data
Relevant demographic and operative data between the PJK and non-PJK groups is summarized in Table 1. The two groups were comparable in terms of the male-to-female ratio (PJK group, 1:18; non-PJK group, 6:31; P=0.27), age distribution (PKJ group, 69.1±7.0 years; non-PJK group, 70.5±8.4 years; P=0.24) and the distribution of surgical technique used (PO, PSO and VCR).
Full table
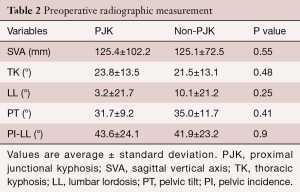
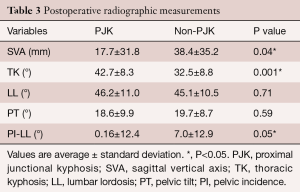
Radiographic measurements
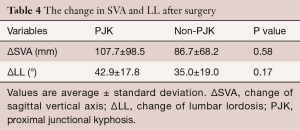
Radiographic measurements were taken pre-operatively and on the first post-operative day when a patient was able to stand. Change in measured radiographic variables from pre-operative baseline is reported in Table 2, and summarized for the PJK and non-PJK group, respectively, as follows: SVA, 125.4 versus 125.1 mm, P=0.55; LL, 3.2° versus 10.1°, P=0.25; TK, 23.8° versus 21.5°, P=0.48; and PT, 31.7° versus 35.0°, P=0.41. Based on the SRS-Schwab classification (5), a clinically acceptable sagittal alignment was achieved in all patients, with SVA measures for the PJK and non-PJK group, respectively, of 17.7 versus 38.4 mm and PI-LL of 0.16° versus 7.0°. The post-operative PT was also comparable between the two groups: PKJ, 18.6°, non-PKJ, 19.7°, P=0.41. Moreover, a clinically acceptable spinopelvic sagittal alignment, according to SRS-Schwab classification, was also achieved in all patients after surgery (Table 3). Change in SVA and LL from baseline for the PJK and non-PJK group, respectively, were as follows: SVA, 107.7 mm versus 86.7 mm, P=0.58; LL, 42.9° versus 35.0°; P=0.17; Table 4). The distribution and grade of PJK is reported in Table 5, and summarized as follows: type 1, 6 patients; type 2, 12 patients; type 3, 1 patient; grade A, 12 patients; grade B, 7 patients; and grade C, 0 patients.
Full table
Full table
Full table

Full table
Patient outcomes and revision surgery
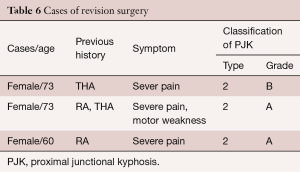
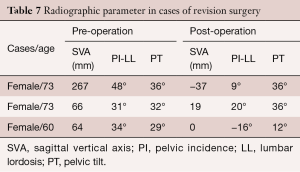
A symptomatic PJK developed in only 3 cases, all of which were classified as type 2, with 2 cases classified as a grade A and 1 case as a grade B. All three cases required revision surgery, at 3, 4 and 18 months, respectively. Of these three cases, two patients had a history of rheumatoid arthritis, with one having undergone a total hip arthroplasty, while the other patient had previously undergone a total hip arthroplasty (Table 6). In both of patients with a history of rheumatoid arthritis, post-operative SVA measures were clinically acceptable, but with a persistent retroversion of the pelvis. For the patient with a history of total hip arthroplasty only, a clinically acceptable sagittal plane alignment had been achieved in terms of SVA, PI-LL and PT measures (Table 7). Revision surgery to extend the fusion to T5 was performed for all three cases, with good clinical outcomes achieved.
Full table
Full table
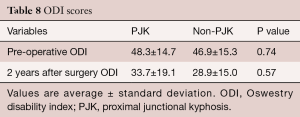
Pre-operative ODI scores were comparable between groups (Table 8): PJK, 48.3; non-PJK (excluded revision cases), 46.9; P=0.74. The ODI scores remained comparable between the two groups at 2 years after surgery: PJK, 33.7; non-PJK (excluded revision cases), 28.9; P=0.57. The ODI scores at 2 years after surgery in type 2 PJK was higher, but not significant, than type 1 PJK: type 2, 41.8; type 1, 29.1; P=0.15.
Full table
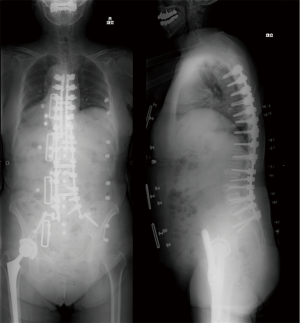
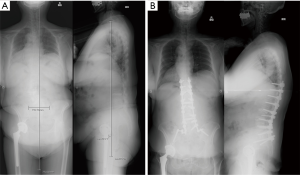
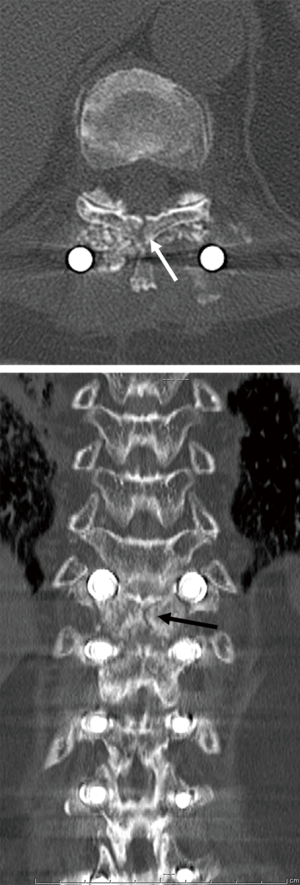
Illustrative case
As an illustrative case, we present the clinical presentation of a 73-year-old female, with a history of rheumatoid arthritis and previous total hip arthroplasty, how underwent spinal fusion from T9/T10 to the ilium. UIV fracture occurred 3 months after corrective surgery, and was associated with lower limb paralysis (Figure 1). Computed tomography revealed a fracture line extending to posterior lamina of the vertebra (Figure 2). As the three-column fracture was unstable, revision surgery was performed, extending the fusion to T5 (Figure 3). Lower limb paralysis recovered gradually after revision surgery.
Discussion
PJK is a common complication of long spinal fusion used in the treatment of adults with spinal deformities (7,8,10,16,19). Although PJK after long spinal fusion has been reported, almost all previous reports included different UIV levels, with a comparable incidence rate of PJK reported for UIVs at proximal and distal thoracic segments (8,21). However, compression fractures were more prevalent among patients developing a PJK of the distal thoracic spine, while subluxation was prevalent among patients who developed a PJK of the proximal thoracic spine. Therefore, the mechanisms contributing to PJK may vary according to UIV level. Therefore, comparisons of the incidence rate and mechanism of PJK after corrective surgery for adult spinal deformity should include only cases using the same levels of fusion.
In our case series, we reported a prevalence rate of PJK of 33.9%, with UIV fracture being the principle underlying cause of PJK. Our incidence rate was comparable to previously reported rates ranging between 20% and 41% (7-17). Although age >55 years has been reported as a risk factor for PJK, we did not identify age as a significant influence in our case series, probably because 96.4% of our patients were over the age of 55 years (mean age, 70 years). Maruo et al. also reported that a pre-operative TK >30° was a specific risk factor for PJK (7). Our case series our analysis did not include the data of patients with a TK >40° as these patients would have required a UIV location in the upper thoracic spine and not at T9/T10, which was the proximal fusion level of interest in our study. This exclusion criterion may explain the comparable TK among patients in both the PJK and non-PJK groups in our study.
Hey et al. reported radiographic study regarding lower thoracic mobility in adult patients (22). They proposed the T9 as a more suitable choice of UIV to fulfill the biomechanical concept of bridge fixation in corrective surgery for adult spinal deformity. However, there was no significant difference in incidence of PJK by UIV (T9: 36.8%, T10: 32.4%) in our study.
Although post-operative SVA and PI-LL measures were significantly lower among patients in the PJK group, compared to those in the non-PJK group, both groups exhibited clinically acceptable spinopelvic alignment after surgery.
Overcorrection of the lumbar curve, which induces a reciprocal change in the curvature of the thoracic spine, increases the mechanical loading on the proximal fusion UIV and, thereby, increases the risk for PJK (7,13,17,23,24). Achieving an optimal LL that is matched to the incidence angle of the pelvis (PI) is, therefore, an important factor for the prevention of PJK (17). However, in our case series, adequate correction of the spinal deformity was achieved in most patients who developed a PJK despite an optimal post-operative sagittal alignment. Therefore, spinopelvic alignment is not a unique risk factor for PJK. There is also some controversy regarding the clinical impact of a PJK. As a PJK is associated with a low incidence rate of neurological consequences and revision surgeries, a number of studies have proposed that PJK is simply a radiological finding with no significant clinical impact (19,25,26). In fact, Yagi et al. also did not identify a significant difference in clinical outcomes among patients with and without a PJK following spinal fusion (9). Moreover, ODI scores were comparable for the PJK and non-PJK groups in our study. Traditionally, PJK has been defined as a change in PJA ≥10° from pre-operative baseline. However, this PJA cutoff does not correspond to clinical symptoms. Therefore, we recommend the use of the more detailed classification, which includes: type of PJA (disc and ligamentous failure, bone failure, or implant/bone interface failure); the PJA grade; and the presence of spondylolisthesis (20). Bridwell et al. reported a more stringent definition, using a change in PJA from pre-operative baseline >20° as the critical angle (24).
Development of a PJK that requires revision surgery is a very important clinical complication. In their case series, Yagi et al. reported a revision surgery rate for patients with a PJK of 12.5% (9). In our case series, the revision rate was 15.8% (3 of 19 patients). It is important to note that the 3 patients who required revision surgery in our case series had a history of rheumatoid arthritis and/or total hip arthroplasty. All 3 patients sustained a severe fracture at the UIV, likely due to increased mechanical loading which may have been enhanced by joint destruction of rheumatoid arthritis. One patient did develop lower limb paralysis as a result of the fracture, with symptoms recovering after revision surgery to extend the fusion to a more proximal segment of the thoracic spine. Three cases are too small sample size to evaluate the influence of lower limb joint disease (osteoarthritis, rheumatoid arthritis) to symptomatic PJK. However, we recommend that assessment of the lower limbs disease be included as a component of the standard post-operative assessment of patients who have undergone a T9/T10 to ilium fusion for correction of a TK.
The limitations of our study need to be acknowledged. The one of the major limitation was lack of BMD dates. Foremost, our sample size was small. However, we do believe that it is more meaningful to investigate a limited number of cases with the same fusion range, rather than comparing outcomes for a range of spinal fusions. Our follow-up period of 2 years can also be interpreted as being relatively short, particularly as a PJK can develop in some patients more than 2 year after surgery. However, previous research has demonstrated that most patients who develop a PJK do so in the early post-operative course.
Conclusions
In our case series, the incidence of PJK was 33.9%, with no effect of PJK on ODI scores. In our series, there was no spinopelvic radiographic factor related to PJK differently from previous reports. Symptomatic PJK developed in only 3 cases, presenting as lower limb dysfunction. Lower limbs dysfunction might be related to symptomatic PJK.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflict of interest to declare.
Ethical Statement: The study was approved the clinical research Ethics Committee of our institution (No. 14-306) and written informed consent was obtained from all patients.
References
- Gill JB, Levin A, Burd T, et al. Corrective osteotomies in spine surgery. J Bone Joint Surg Am 2008;90:2509-20. [Crossref] [PubMed]
- Kim YJ, Bridwell KH, Lenke LG, et al. Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: a minimum 5-year follow-up study. Spine (Phila Pa 1976) 2007;32:2189-97. [Crossref] [PubMed]
- Glassman SD, Bridwell K, Dimar JR, et al. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 2005;30:2024-9. [Crossref] [PubMed]
- Schwab F, Lafage V, Patel A, et al. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976) 2009;34:1828-33. [Crossref] [PubMed]
- Schwab F, Ungar B, Blondel B, et al. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976) 2012;37:1077-82. [Crossref] [PubMed]
- Lafage V, Schwab F, Patel A, et al. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976) 2009;34:E599-606. [Crossref] [PubMed]
- Maruo K, Ha Y, Inoue S, et al. Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976) 2013;38:E1469-76. [Crossref] [PubMed]
- Ha Y, Maruo K, Racine L, et al. Proximal junctional kyphosis and clinical outcomes in adult spinal deformity surgery with fusion from the thoracic spine to the sacrum: a comparison of proximal and distal upper instrumented vertebrae. J Neurosurg Spine 2013;19:360-9. [Crossref] [PubMed]
- Yagi M, Akilah KB, Boachie-Adjei O. Incidence, risk factors and classification of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Spine (Phila Pa 1976) 2011;36:E60-8. [Crossref] [PubMed]
- Kim YJ, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976) 2008;33:2179-84. [Crossref] [PubMed]
- Kim HJ, Yagi M, Nyugen J, et al. Combined anterior-posterior surgery is the most important risk factor for developing proximal junctional kyphosis in idiopathic scoliosis. Clin Orthop Relat Res 2012;470:1633-9. [Crossref] [PubMed]
- Wang J, Zhao Y, Shen B, et al. Risk factor analysis of proximal junctional kyphosis after posterior fusion in patients with idiopathic scoliosis. Injury 2010;41:415-20. [Crossref] [PubMed]
- Yagi M, King AB, Boachie-Adjei O. Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine (Phila Pa 1976) 2012;37:1479-89. [Crossref] [PubMed]
- Kim HJ, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis results in inferior SRS pain subscores in adult deformity patients. Spine (Phila Pa 1976) 2013;38:896-901. [Crossref] [PubMed]
- Mendoza-Lattes S, Ries Z, Gao Y, et al. Proximal junctional kyphosis in adult reconstructive spine surgery results from incomplete restoration of the lumbar lordosis relative to the magnitude of the thoracic kyphosis. Iowa Orthop J 2011;31:199-206. [PubMed]
- Denis F, Sun EC, Winter RB. Incidence and risk factors for proximal and distal junctional kyphosis following surgical treatment for Scheuermann kyphosis: minimum five-year follow-up. Spine (Phila Pa 1976) 2009;34:E729-34. [Crossref] [PubMed]
- Kim HJ, Bridwell KH, Lenke LG, et al. Patients with proximal junctional kyphosis requiring revision surgery have higher postoperative lumbar lordosis and larger sagittal balance corrections. Spine (Phila Pa 1976) 2014;39:E576-80. [Crossref] [PubMed]
- Horton WC, Brown CW, Bridwell KH, et al. Is there an optimal patient stance for obtaining a lateral 36" radiograph? A critical comparison of three techniques. Spine 2005;30:427-33. [Crossref] [PubMed]
- Glattes RC, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976) 2005;30:1643-9. [Crossref] [PubMed]
- Yagi M, Rahm M, Gaines R, et al. Characterization and surgical outcomes of proximal junctional failure in surgically treated patients with adult spinal deformity. Spine (Phila Pa 1976) 2014;39:E607-14. [Crossref] [PubMed]
- Fujimori T, Inoue S, Le H, et al. Long fusion from sacrum to thoracic spine for adult spinal deformity with sagittal imbalance: upper versus lower thoracic spine as site of upper instrumented vertebra. Neurosurg Focus 2014;36:E9. [Crossref] [PubMed]
- Hey HWD, Tan KA, Neo CS, et al. T9 versus T10 as the upper instrumented vertebra for correction of adult deformity-rationale and recommendations. Spine J 2017;17:615-21. [Crossref] [PubMed]
- Kim YJ, Lenke LG, Bridwell KH, et al. Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Spine (Phila Pa 1976) 2007;32:2731-8. [Crossref] [PubMed]
- Bridwell KH, Lenke LG, Cho SK, et al. Proximal junctional kyphosis in primary adult deformity surgery: evaluation of 20 degrees as a critical angle. Neurosurgery 2013;72:899-906. [Crossref] [PubMed]
- Lau D, Clark AJ, Scheer JK, et al. Proximal junctional kyphosis and failure after spinal deformity surgery: a systematic review of the literature as a background to classification development. Spine (Phila Pa 1976) 2014;39:2093-102. [Crossref] [PubMed]
- McClendon J Jr, O'Shaughnessy BA, Sugrue PA, et al. Techniques for operative correction of proximal junctional kyphosis of the upper thoracic spine. Spine (Phila Pa 1976) 2012;37:292-303. [Crossref] [PubMed]