Static and dynamic cervical MRI: two useful exams in cervical myelopathy
Introduction
Magnetic resonance imaging (MRI) of the cervical spine is extremely useful in assessing pathological changes at the spinal cord, vertebrae, discs, ligaments and facet joints (1).
It provides excellent anatomical information about the spinal cord macrostructure and its histopathological changes (2). Nevertheless, in patients affected by symptoms due to cervical spondylosis, multiple findings with spinal cord compression are usually demonstrated with MRI and different surgical options are available.
In this study, we evaluate the findings at the static and dynamic (flexion-extension) cervical MRI in a series of patients affected by “long-tract symptoms”.
Methods
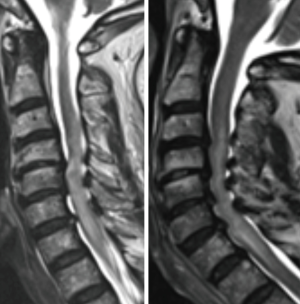
In the period between March 2010 and March 2012, three-hundred-ten patients referred to our department since affected by neck/arm pain or symptoms related to cervical myelopathy. Fifty-eight patients were excluded since affected by tumors, spondylodiscitis, deformity or trauma. Two-hundred-fourteen patients complained neck pain or symptoms related to cervical radiculopathy and were excluded from the study. Thirty-eight patients complained “long-tract symptoms” related to cervical myelopathy. This series of patients was enrolled in the study. All patients underwent clinical and neurological exam. In all the cases, a static and dynamic cervical MRI was executed using a 3.0-T superconducting MR unit (Intera, Philips, Eindhoven, Netherlands). The dynamic exam was performed with as much neck flexion and extension the patient could achieve alone. Custom-built positioning sponges were positioned under the head for flexion and under the shoulder for extension. T1- and T2-weighted sequences were obtained in sagittal and axial plane for the static exam, only T2-weighted images were executed for the dynamic exam. On T2-weigthed MRI each level was assessed independently by two neuroradiologists (example in Figure 1) and Muhle scale was applied (3).
Statistical analysis
All statistical analyses were performed using the PASW Statistics 18 Version 18 (SPSS, Inc., 2009, Chicago, IL, USA).
Results
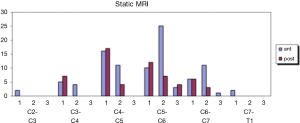
A total of 38 patients were definitively enrolled in the study (Table 1). They were 16 males (42.1%) and 22 females (57.9%), mean age 62.26 (SD =8.72). The symptoms referred were: generalized gait disturbances in 14 cases (36.8%), paresthesia in 7 cases (18.4%), hypoesthesia in 7 cases (18.4%), weakness in 4 cases (10.5%), stiffness in 4 cases (10.5%) and urinary disturbances in 2 cases (5.3%). According to Muhle’s classification of spinal cord compressions static MRI demonstrated 156 findings (Figure 2): 96 (61.54%) anterior and 60 (38.46%) posterior. The anterior compressions were: grade 1 in 41 cases (42.7%), grade 2 in 51 cases (53.12%), grade 3 in 4 cases (4.18%). The posterior compressions were: 42 (70%) of grade 1, 14 (23.3%) of grade 2 and 4 (6.7%) of grade 3.
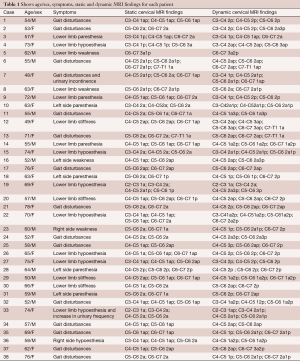
Full table
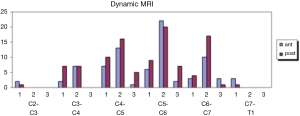
Dynamic MRI showed 186 spinal cord compressions (Figure 3): 81 (43.5%) anterior and 105 (56.5%) posterior. The anterior compressions were: grade 1 in 23 cases (28.4%), grade 2 in 52 cases (64.2%), grade 3 in 6 cases (7.4%). The posterior compressions were: 32 (30.48%) of grade 1, 60 (57.14%) of grade 2, 13 (12.38%) of grade 3.
Discussion
In this study, we report our experience in using the dynamic cervical MRI in addition to the static exam. The dynamic exam was executed in a series of patients affected by long tract symptoms in which there was not a clear surgical plan. The findings at the static and dynamic exam with the relative grade of spinal cord compression are reported.
Muhle proposed a new classification system analysing eighty-one patients with different stages (I–IV) of degenerative disease of the cervical spine examined with MRI. He classified each segment as: 0= normal, 1= partial obliteration of the anterior or posterior subarachnoid space, 2= complete obliteration of subarachnoid space and 3= cervical cord compression or displacement.
The antero-posterior diameter of the spinal canal has been reported to be increased in flexion and decreased in extension (4).
Sayit et al. (5) investigated the dynamic change of the ligamentum flavum in the cervical spine using dynamic MRI. They reported that ligamentum flavum at C7-T1 was significantly thicker than C2-3 to C6-C7. It was significantly thicker in extension than flexion at C3-C4 to C6-C7.
Somatosensory evoked potentials (SSEPs) during dynamic motion of the cervical spine and the efficacy of dynamic SSEPs have been evaluated in patients with cervical spondylotic myelopathy. SSEPs tended to deteriorate after cervical spine extension and the percent latency and amplitude progressively increased during cervical spine extension in these patients (6).
Yu et al. (7) studied 71 patients affected by cervical myelopathy with and without hyperintensity on T2W MRI and the Cobb angle on cervical flexion-extension radiographs. He concluded that increased segmental hyperextension curvature (≥10°) and range of movement (ROM) are risk factors for high intensity lesions on T2W MRI in these patients.
An analysis of extension MRI found an increased number of compression levels in 72% of patients as compared to the findings of static MRI. The interpretation of asymptomatic spinal compressions based exclusively on extension MRI has been warned to be made with caution (8).
Our study demonstrates that dynamic MRI found more spinal cord compression than static MRI (186 vs. 156). The static exam showed a prevalence of anterior compressions (61.54%), while the dynamic one demonstrated prevalence of posterior compressions (56.5%). The posterior compressions in static MRI are in 70% of grade 1, while in dynamic MRI they are in 57.14% of grade 2. Basing on the additional dynamic exams we obtained more radiological information and this helped us in defining the surgical plan. After the acquisition of static T1- and T2-weighted images, only T2-weighted images were performed for the dynamic exam. The positioning of the neck was easily executed using custom-built sponges and the dynamic exam required an acquisition time of a few minutes more (15–20 minutes in total for static and dynamic MRI) with a slightly higher cost. Finally, we consider the dynamic cervical MRI an additional exam with a slightly higher acquisition time and cost, however it adds useful radiological information to the surgical plan. This exam can be particularly useful for the treatment of patients affected by cervical myelopathy, since their neurological exam does not usually give information about the level to operate and many surgical options are available. The high rate of radiological findings in extension images suggests its careful evaluation and integration with flexion images.
Conclusions
Dynamic cervical MRI shows a major number of findings compared to static MRI with a prevalence of posterior ones, which are in 57.14% with complete obliteration of subarachnoid space. Its use in conjunction with static MRI may be useful in patients affected by cervical myelopathy in order to plan the operation, but a careful evaluation of the posterior findings should be done since they are probably overexpressed by dynamic MRI.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by our Institution and written informed consent was obtained from all patients.
References
- Guppy KH, Hawk M, Chakrabarti I, et al. The use of flexion-extension magnetic resonance imaging for evaluating signal intensity changes of the cervical spinal cord. J Neurosurg Spine 2009;10:366-73. [Crossref] [PubMed]
- Zhang C, Das SK, Yang DJ, et al. Application of magnetic resonance imaging in cervical spondylotic myelopathy. World J Radiol 2014;6:826-32. [Crossref] [PubMed]
- Muhle C, Metzner J, Weinert D, et al. Classification system based on kinematic MR imaging in cervical spondylitic myelopathy. AJNR Am J Neuroradiol 1998;19:1763-71. [PubMed]
- Dalbayrak S, Yaman O, Firidin MN, et al. The contribution of cervical dynamic magnetic resonance imaging to the surgical treatment of cervical spondylotic myelopathy. Turk Neurosurg 2015;25:36-42. [PubMed]
- Sayit E, Daubs MD, Aghdasi B, et al. Dynamic changes of the ligamentum flavum in the cervical spine assessed with kinetic magnetic resonance imaging. Global Spine J 2013;3:69-74. [Crossref] [PubMed]
- Morishita Y, Maeda T, Ueta T, et al. Dynamic somatosensory evoked potentials to determine electrophysiological effects on the spinal cord during cervical spine extension: clinical article. J Neurosurg Spine 2013;19:288-92. [Crossref] [PubMed]
- Yu L, Zhang Z, Ding Q, et al. Relationship Between Signal Changes on T2-weighted Magnetic Resonance Images and Cervical Dynamics in Cervical Spondylotic Myelopathy. J Spinal Disord Tech 2015;28:E365-7. [Crossref] [PubMed]
- Kim CH, Chung CK, Kim KJ, et al. Cervical extension magnetic resonance imaging in evaluating cervical spondylotic myelopathy. Acta Neurochir (Wien) 2014;156:259-66. [Crossref] [PubMed]