Different operative findings of cases predicted to be symptomatic discal pseudocysts after percutaneous endoscopic lumbar discectomy
Introduction
Percutaneous endoscopic lumbar discectomy (PELD) is one of the most sophisticated operative procedures for the treatment of lumbar disc herniation (LDH) (1-3). However, the complications of PELD have not been fully reported. Although postoperative discal pseudocyst (PDP) is one of the complications after discectomy, Kang and Park first reported symptomatic PDP after PELD in 2011 (4). In general, PDP is diagnosed on the basis of typical MRI findings [a cystic lesion at the discectomy site, with low intensity of a T1-weighted image (T1WI) and high intensity on a T2-weighted image (T2WI)]; however, intraoperative confirmation was not fully performed in these reported cases (4-6). The reason for continuing conservative treatment is that spontaneous regression may be expected with this pathological condition (4-6).
Symptomatic PDP has to be differentially diagnosed from other cystic lesions such as juxtafacet cysts, perineural cysts, and ganglion cysts. However, there has been no discussion about differential diagnosis of a simple recurrence of LDH in previous reports (4-6). We therefore present a case of recurrent LDH resembling symptomatic PDP and real symptomatic PDP, and further discuss the difficulty of the differential diagnosis.
Case presentation
Case 1
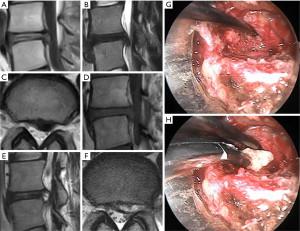
A 27-year-old male patient presented with low back pain and right leg pain that started 2 months before visiting our outpatient clinic. Neurological examination revealed a positive straight-leg rising sign (SLR) at 30° on the left side. Plain lumbar radiographs demonstrated slight narrowing of disc heights. Lumbar magnetic resonance imaging (MRI) revealed a spherical lesion at the L4/5 intervertebral disc level, with marked compression of the left L5 nerve root; the lesion had low intensity on both T1WI and T2WI (Figure 1A-C). We diagnosed LDH and performed PELD with a transforaminal approach. Immediately after the operation, his leg pain improved. He was discharged the day after the operation. Twenty days later, he developed recurrent leg pain. As the pain gradually increased, he visited our outpatient clinic and underwent MRI. MRI revealed a cystic lesion at the operated disc level, with marked compression of left L5 nerve root; the lesion had a low signal intensity on T1WI and high signal intensity on T2WI (Figure 1D-F). We diagnosed symptomatic PDP and performed microendoscopic discectomy to observe the wide area including the surrounding part of the initial operative site. After retraction of the L5 nerve root to the right side, we first confirmed the smooth surface of this cystic lesion (Figure 1G). We expected to observe spouting fluid after puncturing the surface; however, a solid nucleus pulposus appeared (Figures 1H). After the total removal of the nucleus, his leg pain improved and he was discharged 3 days after the operation. Thereafter, he has shown no recurrent leg pain during the 29-month follow-up period.
Case 2
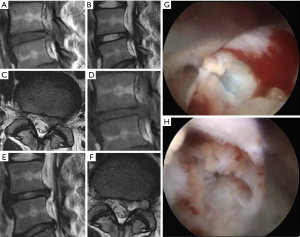
A 14-year-old female patient presented with worsening low back pain and right leg pain that appeared 2 months before visiting our outpatient clinic. Neurological examination revealed slight muscle weakness and a positive SLR at 50° on the left side. Plain lumbar radiographs demonstrated slight narrowing of disc heights. Lumbar MRI revealed a lesion at the L4/5 intervertebral disc level, with marked compression of the left L5 nerve root; the lesion had low intensity on both T1WI and T2WI (Figure 2A-C). We diagnosed LDH and performed PELD with a transforaminal approach. Immediately after the operation, her leg pain was relieved. She was discharged the day after the operation. Thirty days later, she developed recurrent leg pain and visited our outpatient clinic. Because the pain gradually increased, we performed MRI, which revealed a cystic lesion at the operated disc level, with marked compression of the left L5 nerve root; the lesion had a low signal intensity on T1WI and high signal intensity on T2WI (Figure 2D-F). We suspected symptomatic PDP and performed PELD with the same operative route. After reaching the vertebral foramen, we first confirmed the smooth and thin surface of this expanding cystic lesion (Figure 2G). After puncturing the surface, we observed spouting serous fluid and annulus tear on the further side of the cyst (Figures 2H). After the removal of the cyst wall as much as possible, the patient was relieved of her leg pain and discharged the day after the operation. Thereafter, she has shown no recurrent leg pain during the 2-month follow-up period.
Discussion
PDP is one of the complications after discectomy. PDP is also known as postdiscectomy pseudocyst (4) or postoperative annular pseudocyst (6). PDP has extremely similar characteristics to discal cysts except for the history of operative treatment for LDH. Chiba et al. reported the characteristics of discal cysts, as follows: (I) clinical symptoms of a unilateral single nerve root lesion; (II) occurring at a slightly younger age and at higher intervertebral levels than does typical disc herniation; (III) minimal degeneration of the involved disc on imaging evaluations; (IV) presence of a communication between the cyst and corresponding intervertebral discs on discography, with severe radiating pain in the affected leg at the time of injection; (V) a cyst containing bloody to clear serous fluid; and (VI) absence of disc materials or a specific lining cell layer on histological examination (7). MRI has a very high sensitivity in diagnosing discal cysts, and has mostly demonstrated spherical extradural masses with low intensity on T1WI and high intensity on T2WI (8,9).
Although, in our clinical experience, nonsymptomatic PDP is incidentally found on postoperative follow-up MRI, symptomatic PDP is a relatively rare complication. Kang and Park reported that the incidence of symptomatic PDP after PELD was 1.0% in their large series (15 of 1,503 cases) (4). Our experience with PELD is lower than that of Kang and Park; we encountered only one patient with symptomatic PDP among 359 patients from July 2009 to September 2016 (0.28%). Interestingly, we also experienced a case of recurrent LDH mimicking symptomatic PDP. Although MRI is a very useful and noninvasive diagnostic method, a review of 56 cases by Aydin et al. revealed that the signal intensities of discal cysts may not be the diagnostic basis (8). In T1WI, the cyst was hypointense in 68.7%, isointense in 29%, and hyperintense in 2% of the cases. On the other hand, in T2WI, the cyst was hyperintense in 96%, isointense in 2%, and hypointense in 2% of the cases. Gadolinium-diethylenetriamine penta-acetic acid-enhanced MRI evaluations showed rim enhancement in 92% of the cases. Unfortunately, we could not perform enhanced MRI, and even this radiologic modality might not distinguish PDP from recurrent LDH because enhanced MRI also reveals a similar ring enhancement to recurrent LDH (10,11). Discography is an invasive diagnostic technique (12,13); nevertheless, it may provide useful information about the existence of a communication between the disc and the cyst. Thereby, there is some possibility of excluding recurrent LDH mimicking PDP from real PDP.
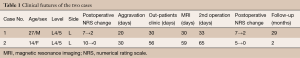
From the viewpoint of clinical features, the differential diagnosis of these pathological conditions is also difficult. The onset of recurrent LDH is expected to be acute; however, the leg pain gradually increased in case 1 (Table 1). A short duration of symptom improvement may indicate the possibility of recurrent LDH, and the duration of case 1 was within the extent of the previously reported cases (20 vs. 9–118 days) (4,5). Spontaneous regression of the lesion may occur in both pathological conditions (5,14,15). The outcome of conservative treatment will not provide additional information about the diagnosis. At present, there is no noninvasive preoperative method to perfectly diagnose symptomatic PDP. Therefore, the possibility of recurrent LDH, even a case demonstrating an expandable round lesion with low intensity on T1WI and high intensity on T2WI, should also be considered.
Full table
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Choi G, Lee SH, Deshpande K, et al. Working channel endoscope in lumbar spine surgery. J Neurosurg Sci 2014;58:77-85. [PubMed]
- Sairyo K, Egawa H, Matsuura T, et al. State of the art: Transforaminal approach for percutaneous endoscopic lumbar discectomy under local anesthesia. J Med Invest 2014;61:217-25. [Crossref] [PubMed]
- Yeung AT. The Evolution and Advancement of Endoscopic Foraminal Surgery: One Surgeon's Experience Incorporating Adjunctive Techologies. SAS J 2007;1:108-17. [Crossref] [PubMed]
- Kang SH, Park SW. Symptomatic post-discectomy pseudocyst after endoscopic lumbar discectomy. J Korean Neurosurg Soc 2011;49:31-6. [Crossref] [PubMed]
- Chung D, Cho DC, Sung JK, et al. Retrospective report of symptomatic postoperative discal pseudocyst after lumbar discectomy. Acta Neurochir (Wien) 2012;154:715-22. [Crossref] [PubMed]
- Young PM, Fenton DS, Czervionke LF. Postoperative annular pseudocyst: report of two cases with an unusual complication after microdiscectomy, and successful treatment by percutaneous aspiration and steroid injection. Spine J 2009;9:e9-15. [Crossref] [PubMed]
- Chiba K, Toyama Y, Matsumoto M, et al. Intraspinal cyst communicating with the intervertebral disc in the lumbar spine: discal cyst. Spine (Phila Pa 1976) 2001;26:2112-8. [Crossref] [PubMed]
- Aydin S, Abuzayed B, Yildirim H, et al. Discal cysts of the lumbar spine: report of five cases and review of the literature. Eur Spine J 2010;19:1621-6. [Crossref] [PubMed]
- Lee HK, Lee DH, Choi CG, et al. Discal cyst of the lumbar spine: MR imaging features. Clin Imaging 2006;30:326-30. [Crossref] [PubMed]
- Białecki J, Lukawski S, Milecki M, et al. Differential diagnosis of post-surgery scars and recurrent lumbar disc herniation in MRI. Ortop Traumatol Rehabil 2004;6:172-6. [PubMed]
- Haughton V, Schreibman K, De Smet A. Contrast between scar and recurrent herniated disk on contrast-enhanced MR images. AJNR Am J Neuroradiol 2002;23:1652-6. [PubMed]
- Marshman LA. Discal cysts. J Neurosurg Spine 2007;7:575-6; author reply 576-7. [Crossref] [PubMed]
- Nabeta M, Yoshimoto H, Sato S, et al. Discal cysts of the lumbar spine. Report of five cases. J Neurosurg Spine 2007;6:85-9. [Crossref] [PubMed]
- Chou D, Smith JS, Chin CT. Spontaneous regression of a discal cyst. Case report. J Neurosurg Spine 2007;6:81-4. [Crossref] [PubMed]
- Takeshima Y, Takahashi T, Hanakita J, et al. Lumbar discal cyst with spontaneous regression and subsequent occurrence of lumbar disc herniation. Neurol Med Chir (Tokyo) 2011;51:809-11. [Crossref] [PubMed]


