Lumbar disc herniation presenting with contralateral symptoms: a case report
Introduction
Lumbar disc herniation is common (1-3) and may be symptomatic (1,4). It usually presents with varying degrees of pain, numbness and weakness in the distribution of the affected nerve root (4,5). Although it is often diagnosed clinically, an MRI is needed to confirm the diagnosis and localize the pathology prior to any forms of intervention (6,7). Contralateral leg symptoms cast doubt on the diagnosis as many herniated discs are asymptomatic (2,3). In such cases, surgery should be avoided.
We report a unique case of left lumbar disc herniation at L5/S1 who presented with right-sided symptoms and successfully treated with a right L5/S1 foraminal block.
Case presentation
A 24-year-old gentleman who worked as a bellboy, presented with a 5-month history of low back pain radiating down his right buttock, posterior thigh and posterior leg. The patient did not recall any inciting trauma. He did not have any associated lower limb paresthesia or weakness, and did not have any bowel or bladder incontinence. Examination revealed weakness in the right flexor hallucis longus of grade 4, with an otherwise normal neurological examination. Straight leg raise was negative bilaterally. Plain X-rays of the lumbar spine was normal. He was managed conservatively with physiotherapy and analgesia.
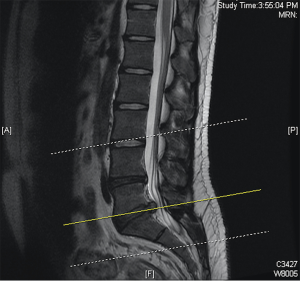
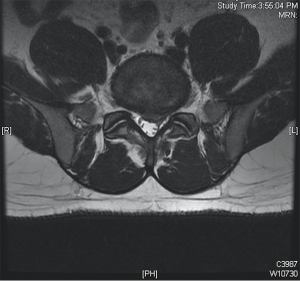
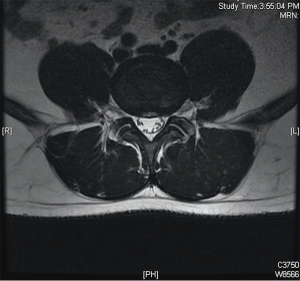
Upon review at 6 weeks, his symptoms did not improve. MRI of his lumbar spine showed a left-sided paracentral disc herniation at L5/S1 causing stenosis of the left lateral recess (Figures 1,2). There was no prolapsed disc seen on the right side or at the L4/5 level despite evidence of disc degeneration (Figure 3). There was no abnormality in the facet joints or the ligamentum flavum.
As the symptoms were on the right side, the patient was counseled for a right L5/S1 foraminal block for both diagnostic and therapeutic purposes. The foraminal block was performed successfully with Shincort and Marcaine in a 1:1 ratio (total 3 mL) under fluoroscopic guidance. He had complete resolution of the pain in his right lower limb and went back to work for the next 6 weeks.
Six weeks after the foraminal block, the patient presented with a 5-day insidious onset of low back pain radiating down his left posterior thigh and leg. This was associated with paresthesia over his left posterior thigh. There was again no precipitating event or inciting trauma. Neurological examination of his lower limbs was normal. Straight leg raise was positive at 40 degrees on the left side.
Given the concordance between his current clinical symptoms and the MRI findings this time, he underwent a left L5/S1 microdiscectomy. A repeat MRI was not performed as there was no precipitating event or inciting trauma during this period. His left leg symptoms resolved completely after the surgery up to 1 year of follow-up.
Discussion
Radiculopathy from lumbar disc herniation can be a result of mechanical compression (8), ischaemia (8) or inflammatory irritation (9) of the nerve root. Surgery may be indicated in selected patients who are refractory to conservative management if leg symptoms are concordant with MRI scans (5). Despite the fact that several cases have been reported in the literature of patients who presented with contralateral leg symptoms (10-12), it remains difficult to recommend surgery in general to these patients with discordant symptoms. To the best of the author’s knowledge, this case is unique because a successful foraminal block delivered on the symptomatic side not only re-localizes the leg symptoms to the side of lesion, but also gave transient relief to the patient’s symptoms. This phenomenon suggests that the disc herniation at L5/S1 is indeed the cause of patient’s symptoms despite being on the contralateral side.
The mechanism for lumbar disc herniation presenting with contralateral leg symptoms is poorly understood (10,11). Kornberg et al. (13) proposed that inconsistent dural attachments to the posterior longitudinal ligaments holds the lumbar nerve roots at certain levels resulting in a more symptomatic traction of the contralateral nerve root. Sucu et al. (10) in his series of 5 patients with paracentral disc herniation, suggested a similar mechanism resulting in compression of the contralateral nerve root against the facet joint. However these mechanisms have not been widely accepted.
In this patient, a steroid injection was preferred for fear of exposing the patient to unnecessary surgical risk at the expense of treating a potentially asymptomatic herniated disc (2,3). Foraminal blocks have been shown to be an effective treatment modality in patients who fail to respond to oral analgesia and physical therapy, despite their unpredictable and usually short duration of action of 2–4 weeks (5,14). They have also been used as a diagnostic tool to guide treatment by isolating the level and the side of nerve root pathology (14).
Given that the foraminal block is a low risk procedure (15) the authors recommend that this form of intervention should be considered prior to embarking on surgery when mismatch between the clinical picture and radiological findings arises. Interestingly, the patient’s symptoms returned on the ipsilateral side of the disc herniation insidiously after 6 weeks. He underwent a left microdiscectomy and had an uneventful recovery with full resolution of his symptoms at 1 year of follow-up.
Conclusions
Patients with lumbar disc herniation may present with radicular symptoms involving the contralateral leg. A foraminal block on the symptomatic side is a low risk procedure, and serves as a good diagnostic and therapeutic tool in the management of these patients. It should be performed before subjecting the patient to surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Jordan J, Konstantinou K, O’Dowd J. Herniated lumbar disc. BMJ Clin Evid 2009;2009.
- Jensen MC, Brant-Zawadzki MN, Obuchowski N, et al. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med 1994;331:69-73. [Crossref] [PubMed]
- Boden SD, Davis DO, Dina TS, et al. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects . A prospective investigation Abnormal Lumbar Magnetic-Resonance Spine Scans of the in Asymptomatic. J Bone Joint Surg Am 1990;72:403-8. [Crossref] [PubMed]
- Benoist M. The natural history of lumbar disc herniation and radiculopathy. Joint Bone Spine 2002;69:155-60. [Crossref] [PubMed]
- North American Spine Society. Clinical Guidelines for Diagnosis and Treatment of Lumbar Disc Herniation with Radiculopathy. 2012:87.
- Schneiderman G, Flannigan B, Kingston S, et al. Magnetic resonance imaging in the diagnosis of disc degeneration: correlation with discography. Spine (Phila Pa 1976) 1987;12:276-81. [Crossref] [PubMed]
- Linson MA, Crowe CH. Comparison of magnetic resonance imaging and lumbar discography in the diagnosis of disc degeneration. Clin Orthop Relat Res 1990.160-3. [PubMed]
- Garfin SR, Rydevik B, Lind B, et al. Spinal nerve root compression. Spine (Phila Pa 1976) 1995;20:1810-20. [Crossref] [PubMed]
- Takahashi H, Wada A, Iida Y, et al. Antimicrobial prophylaxis for spinal surgery. J Orthop Sci 2009;14:40-4. [Crossref] [PubMed]
- Sucu HK, Gelal F. Lumbar disk herniation with contralateral symptoms. Eur Spine J 2006;15:570-4. [Crossref] [PubMed]
- Lu EK, Hastürk E, Korkmaz M, et al. Disc Herniation with Contralateral Symptoms. Eur J Surg 2010;1:11-5.
- Akdeniz T, Kaner T, Tutkan I, et al. Unilateral surgical approach for lumbar disc herniation with contralateral symptoms. J Neurosurg Spine 2012;17:124-7. [Crossref] [PubMed]
- Kornberg M. Sciatica contralateral to lumbar disk herniation. Orthopedics 1994;17:362-4. [PubMed]
- Weiner BK, Fraser RD. Foraminal injection for lateral lumbar disc herniation. J Bone Joint Surg Br 1997;79:804-7. [Crossref] [PubMed]
- Goodman BS, Posecion LW, Mallempati S, et al. Complications and pitfalls of lumbar interlaminar and transforaminal epidural injections. Curr Rev Musculoskelet Med 2008;1:212-22. [Crossref] [PubMed]