Minimising costs in spinal surgery: is group & save testing justified in lumbar decompression surgery?
Introduction
Recent developments in performance measurement and reporting systems in the United Kingdom (UK) National Health Service (NHS) have created new challenges in costing health care services (1). In particular, the introduction of the “National Reference Costing Exercise” (NRCE) has substantively changed the way in which health care cost information is reported and used (2). With an evolving culture directing clinicians to minimise unnecessary costs, many surgeons are reviewing their practice in an attempt to meet targets.
Lumbar microdiscectomy and laminectomy are two of the most common neurosurgical procedures performed worldwide. The primary indication is for relief of symptoms resulting from spinal nerve root compression or spinal canal stenosis (3). Minimally invasive techniques are employed to remove prolapsed lumbar discs using high-resolution surgical microscopes, better instruments, and endoscopes. The procedure is relatively straight forward with patients often discharged from hospital within 48 hours (4). The complications associated with the condition include nerve root injury, cerebrospinal fluid (CSF) leak, infection and haemorrhage (5). Nevertheless, blood loss associated with the procedure is usually less than 100 mL (3,5-8). Whilst a lumbar laminectomy is technically less invasive, resection of bone is usually associated with oozing of blood and may potentially incur slightly more blood loss. Transfusion is usually indicated when procedure related blood loss exceeds 750 mL.
A recent study from Saxena and Eljamel (4) demonstrated that group & save testing was not required for lumbar microdiscectomy, yet this practice still persists in 28 of the 32 UK Neurosurgical centres (4). The Institute of Neurological Sciences, Queen Elizabeth University Hospital, Glasgow routinely practise group & save sampling prior to elective lumbar decompression surgery with an approximate cost of £20.00 per sample.
A series of consecutive patients treated with lumbar microdiscectomy and laminectomy in a large United Kingdom neurosurgical centre is presented in order to ascertain whether pre-operative group and save testing is justified for these cases.
Methods
We hypothesize that despite current practice, pre-operative group and save testing in unnecessary. In order to test this hypothesis we used the following methods.
Patient archives were reviewed to identify patients undergoing primary elective lumbar decompression surgery at the Institute of Neurological Sciences, Queen Elizabeth University Hospital, Glasgow, UK over a three year period.
The health records of all patients were critically reviewed; hematology results before and after surgery, whether group and save was carried out, and blood transfusion requirements, if any, were collected. Operation room records were reviewed for intra-operative details. Particular attention was given to evaluation of pre- and postoperative investigations and management of any blood loss.
For the purpose of this study microdiscectomy patients were classed as those who underwent an elective single level intra-disc procedure, involving fenestration as opposed to laminectomy. Laminectomy patients were those who had posterior decompression only. Cases were excluded when they involved the insertion of permanent fixation devices, revision surgery and where the theatre register was unclear about cases details.
Descriptive statistics were used and Microsoft Excel used to analyse data. An economic analysis of the cost of group and save and postoperative hematology investigations was performed.
Results
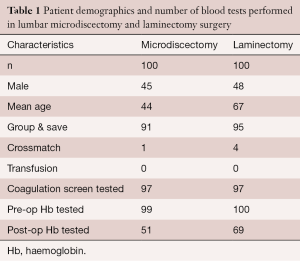
Two hundred patients who had undergone a primary procedure were identified from the operating room records, 100 microdiscectomy and 100 laminectomy (Table 1). The majority of patients were female in both cohorts (55% for microdiscectomy; 52% for laminectomy). The mean age was lower in the microdiscectomy group (44 years) compared to a mean age of 67 years in the laminectomy cohort.
Full table
Ninety-one percent of microdiscectomy patients and 95% of laminectomy patients underwent group and save testing prior to surgery. Interestingly, only one microdiscectomy patient had an acute cross-match performed compared to 5% of laminectomy patients. No patients received a transfusion as a result of their procedure. In total, 97% of patients in both cohorts underwent coagulation testing pre-operatively with 99% of microdiscectomy and all of laminectomy patients having a pre-operative haemoglobin check. Post-operatively 51% in the microdiscectomy group and 69% of patients in the laminectomy group underwent post-operative haemoglobin testing within 48 hours of surgery.
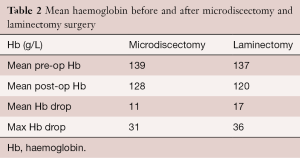
Of those who had a full blood count the mean the mean pre-operative hemoglobin of the microdiscectomy cohort was 139 g/L compared to 128 g/L post operatively. In the laminectomy cohort the pre-operative hemoglobin was 137 g/L compared to 120 g/L post-operatively. The mean hemoglobin drop after surgery was therefore 11 g/L for the microdiscectomy group and 17 g/L for the laminectomy group (Table 2).
Full table
Discussion
Lumbar disc prolapse has become increasingly more common over the past 10 years with lumbar microdiscectomy and laminectomy being two of the most common procedures performed in the various neurosurgical and spinal units in the world. Despite various references alluding to the lack of requirement for group and save testing (4), the culture of testing and post-operative hemoglobin measurements continues. The lack of national or international guidelines allows for an erratic practice, particularly when operations such as microdiscectomy do not feature on the national blood ordering schedule as recommended by the UK national blood transfusion guidelines (9). However, it actually recommends that lumbar laminectomy allows for a group and save sample prior to surgery. Our study supports the findings of Saxena who demonstrated that there was a lack of evidence to support regular group & save testing or post-operative hemoglobin assessment for microdiscectomy. Additionally, to our knowledge this is the first to provide evidence that lumbar laminectomy can also be performed without the tests outlined.
Interestingly, these findings are in the presence of a higher mean age in the laminectomy cohort. In the microdiscectomy cohort, the average drop in haemoglobin was 11 g/L compared to 17 g/L in the laminectomy cohort. This is in keeping with the concept that the oozing from bone will be more problematic than the technical difficulties associated with a more invasive procedure.
Our findings strongly support abandoning the practice of preoperative group and save as well as postoperative hemoglobin measurements in patients undergoing lumbar decompression surgery. The cost of group and save in our cohort was £3,720 and the cost of postoperative blood checks was £4,804. Therefore, avoiding these tests would have saved our institution a total of £8,524 for this cohort.
The potential saving per unit may appear insignificant, but both microdiscectomy and lumbar laminectomy are very common operations, and given that between 1–3% of the population are troubled with herniated discs (10) the potential saving could be quite expansive across the UK.
The argument against extensive testing pre-operatively is based on the logistics of group and save and cross-matching. The standard practice for group and save is to use the gel column technique which takes 30–45 minutes to complete. Cross-matching of serum would only take a few minutes following group and save. Therefore, if blood was required during surgery, cross-matching would only take approximately 60 minutes from requesting blood to delivery. The maximum surgical blood order schedule in the UK is a list of common elective surgical procedures performed with a maximum number of units of blood crossmatched preoperatively for each procedure (11). This gives a guide as to the risk of transfusion for many index procedures.
Resistance to abandonment of these unnecessary procedures prior to surgery has been encountered in other specialties, despite good evidence to suggest the expenditure is necessary (12-14). This is probably due to concerns regarding catastrophic intra-operative blood loss in very rare circumstances. In these cases, however, the presence of O negative blood in the theater emergency fridge should always be available.
Conclusions
Our findings strongly suggest that pre-operative group and save is unnecessary in lumbar microdiscectomy and laminectomy. As such, we support the abandonment of routine pre-operative group and save testing and post-operative blood checks. However, a reserve stock of O negative blood should be available in case of major peri-operative bleeding.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Sprinks J. Lord Carter's model hospitals aim to save the NHS £5 billion a year. Nurs Stand 2016;30:12-3.
- Department of Health. National Reference Costing Exercise. 2016. Available online: www.gov.uk
- Palmer S. Use of a tubular retractor system in microscopic lumbar discectomy: 1 year prospective results in 135 patients. Neurosurg Focus 2002;13:E5. [Crossref] [PubMed]
- Saxena A, Eljamel S. Preoperative "group and save" in lumbar microdiscectomy: is it necessary? J Neurosurg Spine 2011;15:686-8. [Crossref] [PubMed]
- German JW, Adamo MA, Hoppenot RG, et al. Perioperative results following lumbar discectomy: comparison of minimally invasive discectomy and standard microdiscectomy. Neurosurg Focus 2008;25:E20. [Crossref] [PubMed]
- Righesso O, Falavigna A, Avanzi O. Comparison of open discectomy with microendoscopic discectomy in lumbar disc herniations: results of a randomized controlled trial. Neurosurgery 2007;61:545-9; discussion 549. [Crossref] [PubMed]
- Ryang YM, Oertel MF, Mayfrank L, et al. Standard open microdiscectomy versus minimal access trocar microdiscectomy: results of a prospective randomized study. Neurosurgery 2008;62:174-81; discussion 181-2. [Crossref] [PubMed]
- Huang TJ, Hsu RW, Li YY, et al. Less systemic cytokine response in patients following microendoscopic versus open lumbar discectomy. J Orthop Res 2005;23:406-11. [Crossref] [PubMed]
- National Blood Transfusion Committee: Guidelines for the Blood Transfusion Services in the United Kingdom, 7th Edition. UK Blood Transfusion & Tissue Transplantation Services. Available online: http://www.transfusionguidelines.org.uk
- Andersson G. Epidemiology of spinal disorders. In: Frymoyer JW, Ducker TB, Hadler NM, et al. editors. The adult spine: principles and practice. New York, NY: Raven Press, 1997:93-141.
- Hardy NM, Bolen FH, Shatney CH. Maximum surgical blood order schedule reduces hospital costs. Am Surg 1987;53:223-5. [PubMed]
- Quinn M, Suttie S, Li A, et al. Are blood group and save samples needed for cholecystectomy? Surg Endosc 2011;25:2505-8. [Crossref] [PubMed]
- Hamza N, Pereira M, Gilliam A. Routine ‘group and save’ is unnecessary on the day of surgery for elective laparoscopic cholecystectomy. The Bulletin of the Royal College of Surgeons of England 2015;97:E1-4. [Crossref]
- Malik H, Bishop H, Winstanley J. Audit of blood transfusion in elective breast cancer surgery--do we need to group and save pre-operatively? Ann R Coll Surg Engl 2008;90:472-3. [Crossref] [PubMed]
Contributions: (I) Conception and design: WT Wilson, P Fivey; (II) Administrative support: WT Wilson; (III) Provision of study materials or patients: P Fivey; (IV) Collection and assembly of data: WT Wilson, P Fivey; (V) Data analysis and interpretation: WT Wilson, AM Young; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors.


