Clinical presentation and surgical outcomes of an intramedullary C2 spinal cord cavernoma: a case report and review of the relevant literature
Introduction
Spinal cord intramedullary cavernomas (SCICs) are rare, vascular malformations comprised of an enlarged mass of sinusoidal-type vessels lined with a single endothelial layer (1,2). Unlike their intracranial counterpart, SCICs are more likely to give rise to significant neurological findings and are associated with mass effect, myelopathy, hemorrhage and significant morbidity (1,3-5). The clinical presentation varies depending on site, with the thoracic (58%) and cervical (38%) spinal cord being the most frequent locations (3,6). Most patients present with progressive neurological decline, with sensory deficits and motor weakness being the most common presenting symptoms (3,6).
Case presentation
A 56-year-old male presented with sensory changes in his right hand which progressed over a period of weeks to bilateral sensory changes in the upper and lower limbs, gait imbalance, urinary and faecal incontinence and loss of temperature perception. He subsequently developed significant weakness in the upper limbs. Preoperative magnetic resonance imaging (MRI) of the cervical spine (Figure 1) was suggestive of a SCIC and given his rapid neurological decline, a surgical approach to therapy was adopted.
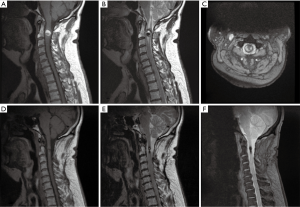
Immediately postoperatively, dense hemiparesis was noted on the right side, however, there was steady improvement in both motor and sensory function over the subsequent days in addition to a complete return of bladder and bowel function. No postoperative complications were noted. Histopathology (Figure 2), consistent with SCICs with hemorrhage, displayed areas of tissue with increased vascularity and characteristic thin walled blood vessels of various sizes. A MRI (Figure 1) was obtained 11 months postoperatively and showed reduced mass effect and resolved spinal cord oedema. The patient continued to demonstrate slow but steady improvement at all postoperative follow-ups.

Discussion
SCICs are rare, representing 5–12% of all spinal vascular diseases and approximately 5% of all spinal cord lesions (1,7,8). The mean incidence of symptomatic presentation and diagnosis is usually in the 3rd to 4th decade of life and the clinical presentation includes two primary patterns: slow-progressive and acute neurological decline, with the former being more common (2,3,6,8). Gross et al. reviewed the clinical presentation of 17 case series and concluded that 65% of patients had at least one sensory deficit, 63% presented with motor weakness and at least 27% of patients had pain (6).
This case is atypical for a number of reasons. Firstly, at 56 years of age, the patient was 14 years above the average age of presentation (42 years) based on the 27 series and 305 patients reviewed by Gross et al. (6). Secondly, the patient presented with features of both a slow-progressive and acute neurological decline—a presenting pattern that is not commonly noted. In fact, of the 205 patients reviewed by Gross et al., variation in the rapidity of neurological decline within a single patient was not reported (6). Compared to the median duration of symptoms prior to admission (12 months) reported by Kivelev et al., our patient had a relatively shorter period of slow progression (6 months) followed by an acute neurological decline in the days prior to surgery (7).
Interestingly, in this case, the patient displayed all previously reported clinical symptoms including motor weakness, sensory deficits and bladder and bowel dysfunction. Given the implications of incontinence in both clinical and social contexts, this symptom often causes patients significant distress in the longer term. According to Gross et al., only 11% of cases had bladder or bowel instability (6). Furthermore, there is a lack of reports noting recovery of bladder function postoperatively (7). In a study by Kivelev et al. of the five patients with existing micturition disorders prior to surgery, no patient experienced significant improvement postoperatively (7). In contrast, our patient had a postoperative return to normal bladder and bowel function. Additionally, our patient showed improvement in both sensory and motor deficits as well as in his gait imbalance. At 18 months postoperatively he had mild dysaesthesia in the right hand which is well controlled with pregabalin, and does not interfere with occupational duties. This contrasts with prior studies that have found that patients with preoperative sensory neurological deficits improved more slowly and less frequently than those with motor neurological deficits (6).
Conclusions
SCICs, although rare, can cause significant neurological deficit and morbidity. Surgical excision can provide significant benefit, including restoration of bladder and bowel function and a rapid recovery for patients who present with sensory neurological deficits. Furthermore, this case highlights that although surgery can provide significant benefit in those presenting with a rapid neurological decline, early surgical management should be considered in patients with a slowly progressive course in order to avoid the risk of subsequent rapid deterioration with persistent neurological deficit.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Seeking formal ethics approval was not considered necessary for this case report due to the fact that this was a review of the patient’s regular scheduled clinical follow-ups and necessary medical imaging. All images and patient details are completely de-identified.
References
- Lu DC, Lawton MT. Clinical presentation and surgical management of intramedullary spinal cord cavernous malformations. Neurosurg Focus 2010;29:E12. [Crossref] [PubMed]
- See-Sebastian EH, Marks ER. Spinal cord intramedullary cavernoma: A case report. W V Med J 2013;109:28-30. [PubMed]
- Babu R, Owens TR, Karikari IO, et al. Spinal cavernous and capillary hemangiomas in adults. Spine (Phila Pa 1976) 2013;38:E423-30. [Crossref] [PubMed]
- Hegde A, Mohan S, Tan KK, et al. Spinal cavernous malformations: magnetic resonance imaging and associated findings. Singapore Med J 2012;53:582-6. [PubMed]
- Bian LG, Bertalanffy H, Sun QF, et al. Intramedullary cavernous malformations: clinical features and surgical technique via hemilaminectomy. Clin Neurol Neurosurg 2009;111:511-7. [Crossref] [PubMed]
- Gross BA, Du R, Popp AJ, et al. Intramedullary spinal cord cavernous malformations. Neurosurg Focus 2010;29:E14. [Crossref] [PubMed]
- Kivelev J, Niemelä M, Hernesniemi J. Outcome after microsurgery in 14 patients with spinal cavernomas and review of the literature. J Neurosurg Spine 2010;13:524-34. [Crossref] [PubMed]
- Liang JT, Bao YH, Zhang HQ, et al. Management and prognosis of symptomatic patients with intramedullary spinal cord cavernoma: clinical article. J Neurosurg Spine 2011;15:447-56. [Crossref] [PubMed]


