Interspinous process spacers versus traditional decompression for lumbar spinal stenosis: systematic review and meta-analysis
Introduction
With the increasingly elderly patient population, the prevalence of degenerative spinal diseases is also rising steadily (1). In lumbar spinal stenosis, the dural sac and nerve roots are often compressed by one or a combination of bulging intervertebral discs, facet joint hypertrophy, and ligamentum flavum hypertrophy (2-5). Many individuals are symptomatic with pain and neurogenic claudication, and may present with muscular weakness, sensory changes and impeded mobility. In the case of lumbar spinal stenosis, for those refractory to conservative or medical therapy, the traditional surgical approach has been bony decompression, such as via a laminectomy using an open or minimally invasive access (6).
Since its introduction over 50 years ago by Knowles (7), interspinous process devices (IPD) or spacers have been designed and tested in various studies as an alternative or adjunct option to traditional decompression surgery (8-11). The rationale for using IPD is that it has been demonstrated that symptoms of lumbar spinal stenosis are often relieved on flexion and exacerbated on extension. IPD devices can limit extension of the spine, which may help relieve pain or neurogenic claudication. Other purported advantages of IPD include improved interlaminar space at the stenosed spinal level (12,13), distraction of interspinous space (14,15), reduced surgical trauma and complications, as well as minimized disruption to the structural integrity of the spine and paraspinal structures. Current IPD spacers on the market include X-Stop® (Medtronic Spine, LLC, CA, USA), Coflex® (Paradigm Spine, LLC, NY, USA), and Superion.
However, the use of interspinous devices is still debated, with recent reports demonstrating a significantly higher reoperation rate (16) with IPD as well as unfavorable cost-effectiveness (17) compared to traditional decompression techniques. Whether there are added benefits of using IPD spacers over the gold standard decompression surgical approach is still being debated. We aimed to conduct a systematic review and meta-analysis of the current literature to assess the relative benefits and risks of interspinous process spacers compared to traditional surgical decompression.
Methods
Literature search strategy
The present review was conducted according to PRISMA guidelines (18) and recommendations (19,20). Electronic searches were performed using Ovid Medline, PubMed, Cochrane Central Register of Controlled Trials (CCTR), Cochrane Database of Systematic Reviews (CDSR), ACP Journal Club and Database of Abstracts of Review of Effectiveness (DARE) from their dates of inception to December 2015. To achieve maximum sensitivity of the search strategy and identify all studies, we combined the terms: “lumbar spinal stenosis”, “interspinous spacer”, “IPD”, “X-Stop”, “Coflex”, “DIAM”, “Wallis”, “Asperius”, “decompression” or “laminectomy” as either keywords or MeSH terms. The reference lists of all retrieved articles were reviewed for further identification of potentially relevant studies. All identified articles were systematically assessed using the inclusion and exclusion criteria.
Selection criteria
Eligible randomized controlled trials (RCTs) or prospective observational studies (OS) for the present systematic review and meta-analysis included those in which patient cohorts underwent treatment for lumbar spinal stenosis using either an interspinous spacer or traditional decompression surgery. When institutions published duplicate studies with accumulating numbers of patients or increased lengths of follow-up, only the most complete reports were included for quantitative assessment at each time interval. All publications were limited to those involving human subjects and in the English language. Abstracts, case reports, conference presentations, editorials and expert opinions were excluded. Review articles were omitted because of potential publication bias and duplication of results.
Data extraction and critical appraisal
All data was extracted from article texts, tables and figures. Two investigators independently reviewed each retrieved article (K.P., P.J.R.). Discrepancies between the two reviewers were resolved by discussion and consensus with senior investigators. Collected data included the publication date, study design, sample size, follow-up duration, interventions, complications, incidence of reoperation, and clinical outcomes, including low back pain, leg pain, the Oswestry disability index (ODI), and the Roland disability questionnaire (RDQ).
Statistical analysis
The risk ratio (RR) and standardized mean difference (SMD) were used as summary statistics. In the present study, both fixed- and random-effects models were tested. In the fixed-effect model, it was assumed that treatment effect in each study was the same, whereas in a random-effects model, it was assumed that there were variations between studies. χ2 tests were used to study heterogeneity between trials. I2 statistic was used to estimate the percentage of total variation across studies, owing to heterogeneity rather than chance, with values greater than 50% considered as substantial heterogeneity. I2 can be calculated as: I2 = 100% × (Q – df)/Q, with Q defined as Cochrane’s heterogeneity statistics and df defined as degree of freedom. If there was substantial heterogeneity, the possible clinical and methodological reasons for this were explored qualitatively. In the present meta-analysis, the results using the random-effects model were presented to take into account the possible clinical diversity and methodological variation between studies. Specific analyses considering confounding factors were not possible because raw data was not available. All P values were 2-sided. All statistical analyses were conducted with Review Manager Version 5.3.2 (Cochrane Collaboration, Software Update, Oxford, UK).
Results
Literature search
A total of 556 references were identified through electronic database searches. After exclusion of duplicate or irrelevant references, 538 potentially relevant articles were retrieved. After detailed evaluation of these articles, 33 articles remained for assessment. After applying selection criteria, 11 studies (16,21-30) were selected for analysis. The study characteristics are summarized in Table 1.
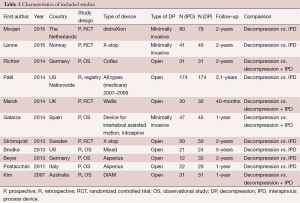
Full table
Baseline characteristics
Similar baseline characteristics were observed in both comparison arms (Table 2). Median age for both IPD and decompression was 67 years (range, 38.5–75 years) and 67 years (range, 42.5–73 years), respectively. The proportion of males in the IPD group was 51.3% (range, 36.7–67%) compared to 48% (range, 27–58%) in the decompression group. The stenosis was localized in IPD patients to L2/3, L3/4, L4/5 at 3%, 17% and 69%, respectively. In the decompression group, the stenosis was localized to L2/3, L3/4, L4/5 in 4%, 18%, and 66% of patients, respectively. Median baseline Visual Analog Scale (VAS) low back pain score was similar between the IPD and decompression cohorts (median 6 each). VAS leg pain scores were also similar (6.1 vs. 6.45), as well as baseline ODI (48.9 vs. 51.8). Surgery time was reported in studies. Lønne et al. reported operating time of 47 minutes in the IPD group versus 113 minutes in the traditional decompression group. Galarza reported 22 minutes surgery time for IPD + decompression compared to 17 minutes for decompression alone, whilst Strömqvist et al. reported IPD surgery time of 62 minutes compared to 98 minutes for decompression.
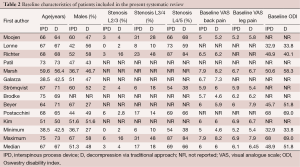
Full table
Assessment of clinical outcomes
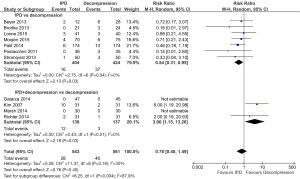
Clinical outcomes were assessed using VAS scores and ODI, assessed into subgroups: studies which compared IPD + decompression vs. decompression, or IPD alone vs. decompression. In terms of VAS scores for low back pain, significantly lower scores were obtained in the decompression group compared to IPD postoperatively (MD, 0.82; 95% CI, 0.61–1.03; I2=3%; P<0.00001). However, IPD as an adjunct to decompression compared with decompression alone resulted in comparable follow-up VAS back pain scores (MD, −0.15; 95% CI, −0.97 to 0.67; I2=66%; P=0.73) (Figure 1).

For VAS leg pain scores, no difference was found between IPD alone versus decompression approaches (MD, 0.18; 95% CI, −1.04 to 1.39; I2=95%; P=0.78). Similarly, there was no difference in postoperative VAS leg pain scores between patients who received both IPD and decompression compared with decompression alone (MD 0.38; 95% CI, −0.12 to 0.88; I2=NA; P=NA) (Figure 1).
There were 2 studies which reported ODI scores for IPD versus decompression. No significant difference was found (MD, −0.32; 95% CI, −2.72 to 2.07; I2=97%; P=0.79). There were also two studies which reported ODI outcomes for IPD+decompression compared with decompression alone. Similarly, there was no significant difference in ODI outcomes at follow-up (MD, 0.28; 95% CI, −0.08 to 0.64; I2=0%; P=0.12) (Figure 1).
Assessment of surgical complications
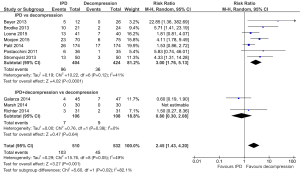
A significantly lower rate of surgical complications was found in the IPD alone group compared to decompression surgery (4.0% vs. 8.7%; RR, 0.54; 95% CI, 0.31–0.95; I2=0%; P=0.03). However, IPD as an adjunct to decompression had significantly higher surgical complications compared to decompression surgery alone (8.6% vs. 2.2%; RR, 3.90; 95% CI, 1.15–13.26; I2=0%; P=0.03) (Figure 2).
Assessment of reoperation rates
IPD was associated with significantly higher reoperation rates compared to decompression (23.7% vs. 8.5%; RR, 3.00; 95% CI, 1.76–5.13; I2=41%; P<0.0001). No significant difference in reoperation rates was found between IPD + decompression cohort versus decompression alone (6.6% vs. 8.3%; RR, 0.80; 95% CI, 0.30–2.08; I2=0%; P=0.64) (Figure 3).
Literature review of costs associated with IPD and decompression
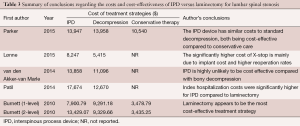
Five studies compared costs associated with IPD versus decompression procedures for lumbar spinal stenosis. Parker et al. developed a Markov model to compare IPD versus decompression vs. conservative care. The authors used data from the Superion FDA clinical trial, a prospective spinal registry, to populate the model, and concluded that IPD device had similar costs to standard decompression. Both were more cost-effective compared to conservative care. Lønne et al. enrolled 96 patients and calculated the cost-effectiveness of X-Stop with minimally invasive decompression for lumbar spinal stenosis. The authors concluded that there is a 50% likelihood that X-stop is cost-effective at the extra cost of €25,700 (incremental cost-effectiveness ratio) for a quality-adjusted life-year. The significantly higher cost of X-stop is mainly due to implant cost and the significantly higher reoperation rate. Van den Akker-van Marle et al., Patil et al., and Burnett et al. made similarly conclusions, with higher costs associated with IPD compared to decompression surgery (Table 3).
Full table
Discussion
Pooled results in the present meta-analysis demonstrate no significant difference in patient-rated clinical outcomes (VAS and ODI scores) between those who receive decompression alone versus standalone IPD or IPD as an adjunct to decompression. There were significantly lower surgical complications associated with implanting a standalone IPD compared to bony decompressive surgery. However, the reoperation rates for standalone IPD were significantly higher than that compared to traditional decompression. These results support prior prospective studies and the conventional belief interspinous spacers may have fewer surgical complications compared to traditional laminectomy, at higher risk of reoperations.
Several randomized trials have compared X-Stop IPD versus standard decompression. In 2013, Strömqvist et al. (16) compared 100 patients with symptomatic one- or two-level lumbar spinal stenosis and neurogenic claudication that was relieved on flexion. Intention-to-treat analysis at 6, 12, 24 months demonstrated no significant differences between X-Stop versus decompression in terms of VAS back pain, VAS leg pain, SF-36 and Zurich Claudication Questionnaire (ZCQ) scores. Reoperation rate for IPD was 26% compared to 6% in the decompression group, which is similar to the pooled results of the present study. There was also an apparent decrease in surgical operation duration (62 vs. 98 minutes) and blood loss (54 vs. 262 mL) for the X-Stop group compared to decompression surgery. A randomized comparison between X-Stop and decompression was also reported by Lønne et al. (22) in 2015. Whilst no differences in patient-reported scores and ZCQ was reported, reoperation rates were significantly higher for IPD versus decompression (25% vs. 5%).
The purported advantages of interspinous or interlaminar stabilization devices are that they distract the spinous processes (14,15) or laminar space and restrict extension. In doing so, these spacers may assist in unloading facet joints, restoration of foraminal height (12,13), and lowering intradiscal pressures (31-33). Initial IPD spacers were designed with the aim of limiting spinal extension, thereby limiting pain and neurogenic claudication (34,35). Devices were also designed with increased rigidity (36) to increase longer-lasting effect. Theoretically, these devices may enlarge neural foramen and decompress nerve roots in patients with spinal stenosis and neurogenic claudication. Depending on the type of interspinous implant used, the procedure is considered minimally invasive. Biomechanically, IPD spacers have been reported to demonstrate non-rigid fixation and can return a destabilized specimen back to the intact state in terms of flexion and extension (37,38). As such, IPD is conventionally thought to be a suitable operation for frail, elderly patients who are at high risk of medical complications compared to open laminectomy.
There are several reported disadvantages associated with IPD devices. In contrast to laminectomy, implantation of interspinous or interlaminar spacers converts the spinous processes from naturally tension-bearing structures to compression-loading structures. This can induce spinous process fractures, an uncommon but recognized complication following IPD implantation. Osteopenic or osteoporotic patients may be particularly susceptible to spinous process fractures. Other studies have reported heterotopic bone formation as a long-term complication following IPD implantation (39). Formation of large osteophytes may intrude into the spinal canal, leading to recurrence of lumbar spinal stenosis symptoms. Tian et al. (40) reported an 81.2% incidence of heterotopic bone formation in 32 patients at 24–57 months follow-up after IPD implantation. Other early complications following IPD implantation include device dislocation and malposition, spinous process erosion, infection, hematoma, and neurological sequelae. A further disadvantage of IPD devices is the poor cost-effectiveness compared to traditional decompression surgery based on current literature reports (17,24,41-43) (Table 3). Based on the current data, the role of IPD spacers remains questionable, given that they do not produce better clinical outcomes, have higher reoperation rates and are more costly compared to traditional decompression surgery.
Limitations
The present systematic review and meta-analysis is constrained by several limitations. It is not valid to extrapolate results to all cases of lumbar spinal stenosis patients. Current evidence has been attained from different brands and types of IPD devices, as such it is difficult to compare efficacy and complication rates between different devices. IPD devices also vary by their mechanism, static versus dynamic, and vary in material composition including titanium, PEEK, and elastomeric substances. The question of which patient subgroup benefits the most from an IPD compared to laminectomy or traditional decompression remains unclear. Future trials should stratify patients according to age groups and comorbidities.
Conclusions
Current evidence indicates no superiority for mid- to long- term patient-reported outcomes for IPD compared with traditional bony decompression, with lesser surgical complications but at the risk of significantly higher reoperation rates and costs. The role of IPD as standalone or adjunct devices for lumbar spinal stenosis surgery needs to be scrutinized, with careful consideration of the risks, benefits and costs before implantation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Hicks GE, Morone N, Weiner DK. Degenerative lumbar disc and facet disease in older adults: prevalence and clinical correlates. Spine (Phila Pa 1976) 2009;34:1301-6. [Crossref] [PubMed]
- Urban JP, Roberts S. Degeneration of the intervertebral disc. Arthritis Res Ther 2003;5:120-30. [Crossref] [PubMed]
- Cinotti G, De Santis P, Nofroni I, et al. Stenosis of lumbar intervertebral foramen: anatomic study on predisposing factors. Spine (Phila Pa 1976) 2002;27:223-9. [Crossref] [PubMed]
- Kandel R, Roberts S, Urban JP. Tissue engineering and the intervertebral disc: the challenges. Eur Spine J 2008;17:480-91. [Crossref] [PubMed]
- Omlor GW, Lorenz H, Engelleiter K, et al. Changes in gene expression and protein distribution at different stages of mechanically induced disc degeneration--an in vivo study on the New Zealand white rabbit. J Orthop Res 2006;24:385-92. [Crossref] [PubMed]
- Phan K, Mobbs RJ. Minimally Invasive Versus Open Laminectomy for Lumbar Stenosis: A Systematic Review and Meta-Analysis. Spine (Phila Pa 1976) 2016;41:E91-E100. [Crossref] [PubMed]
- Gazzeri R, Galarza M, Alfieri A. Controversies about interspinous process devices in the treatment of degenerative lumbar spine diseases: past, present, and future. Biomed Res Int 2014;2014:975052.
- Alfieri A, Gazzeri R, Prell J, et al. Role of lumbar interspinous distraction on the neural elements. Neurosurg Rev 2012;35:477-84; discussion 484. [Crossref] [PubMed]
- Caserta S, La Maida GA, Misaggi B, et al. Elastic stabilization alone or combined with rigid fusion in spinal surgery: a biomechanical study and clinical experience based on 82 cases. Eur Spine J 2002;11 Suppl 2:S192-7. [PubMed]
- Galarza M, Fabrizi AP, Maina R, et al. Degenerative lumbar spinal stenosis with neurogenic intermittent claudication and treatment with the Aperius PercLID System: a preliminary report. Neurosurg Focus 2010;28:E3. [Crossref] [PubMed]
- Sobottke R, Schlüter-Brust K, Kaulhausen T, et al. Interspinous implants (X Stop, Wallis, Diam) for the treatment of LSS: is there a correlation between radiological parameters and clinical outcome? Eur Spine J 2009;18:1494-503. [Crossref] [PubMed]
- Richards JC, Majumdar S, Lindsey DP, et al. The treatment mechanism of an interspinous process implant for lumbar neurogenic intermittent claudication. Spine (Phila Pa 1976) 2005;30:744-9. [Crossref] [PubMed]
- Lee J, Hida K, Seki T, et al. An interspinous process distractor (X STOP) for lumbar spinal stenosis in elderly patients: preliminary experiences in 10 consecutive cases. J Spinal Disord Tech 2004;17:72-7; discussion 78. [Crossref] [PubMed]
- Zucherman JF, Hsu KY, Hartjen CA, et al. A multicenter, prospective, randomized trial evaluating the X STOP interspinous process decompression system for the treatment of neurogenic intermittent claudication: two-year follow-up results. Spine (Phila Pa 1976) 2005;30:1351-8. [Crossref] [PubMed]
- Kondrashov DG, Hannibal M, Hsu KY, et al. Interspinous process decompression with the X-STOP device for lumbar spinal stenosis: a 4-year follow-up study. J Spinal Disord Tech 2006;19:323-7. [Crossref] [PubMed]
- Strömqvist BH, Berg S, Gerdhem P, et al. X-stop versus decompressive surgery for lumbar neurogenic intermittent claudication: randomized controlled trial with 2-year follow-up. Spine (Phila Pa 1976) 2013;38:1436-42. [Crossref] [PubMed]
- Lønne G, Johnsen LG, Aas E, et al. Comparing cost-effectiveness of X-Stop with minimally invasive decompression in lumbar spinal stenosis: a randomized controlled trial. Spine (Phila Pa 1976) 2015;40:514-20. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006-12. [Crossref] [PubMed]
- Phan K, Tian DH, Cao C, et al. Systematic review and meta-analysis: techniques and a guide for the academic surgeon. Ann Cardiothorac Surg 2015;4:112-22. [PubMed]
- Phan K, Mobbs RJ. Systematic reviews and meta-analyses in spine surgery, neurosurgery and orthopedics: guidelines for the surgeon scientist. J Spine Surg 2015;1:19-27.
- Moojen WA, Arts MP, Jacobs WC, et al. IPD without bony decompression versus conventional surgical decompression for lumbar spinal stenosis: 2-year results of a double-blind randomized controlled trial. Eur Spine J 2015;24:2295-305. [Crossref] [PubMed]
- Lønne G, Johnsen LG, Rossvoll I, et al. Minimally invasive decompression versus x-stop in lumbar spinal stenosis: a randomized controlled multicenter study. Spine (Phila Pa 1976) 2015;40:77-85. [Crossref] [PubMed]
- Richter A, Halm HF, Hauck M, et al. Two-year follow-up after decompressive surgery with and without implantation of an interspinous device for lumbar spinal stenosis: a prospective controlled study. J Spinal Disord Tech 2014;27:336-41. [Crossref] [PubMed]
- Patil CG, Sarmiento JM, Ugiliweneza B, et al. Interspinous device versus laminectomy for lumbar spinal stenosis: a comparative effectiveness study. Spine J 2014;14:1484-92. [Crossref] [PubMed]
- Marsh GD, Mahir S, Leyte A. A prospective randomised controlled trial to assess the efficacy of dynamic stabilisation of the lumbar spine with the Wallis ligament. Eur Spine J 2014;23:2156-60. [Crossref] [PubMed]
- Galarza M, Gazzeri R, De la Rosa P, et al. Microdiscectomy with and without insertion of interspinous device for herniated disc at the L5-S1 level. J Clin Neurosci 2014;21:1934-9. [Crossref] [PubMed]
- Brodke DS, Annis P, Lawrence BD, et al. Reoperation and revision rates of 3 surgical treatment methods for lumbar stenosis associated with degenerative scoliosis and spondylolisthesis. Spine (Phila Pa 1976) 2013;38:2287-94. [Crossref] [PubMed]
- Beyer F, Yagdiran A, Neu P, et al. Percutaneous interspinous spacer versus open decompression: a 2-year follow-up of clinical outcome and quality of life. Eur Spine J 2013;22:2015-21. [Crossref] [PubMed]
- Postacchini R, Ferrari E, Cinotti G, et al. Aperius interspinous implant versus open surgical decompression in lumbar spinal stenosis. Spine J 2011;11:933-9. [Crossref] [PubMed]
- Kim KA, McDonald M, Pik JH, et al. Dynamic intraspinous spacer technology for posterior stabilization: case-control study on the safety, sagittal angulation, and pain outcome at 1-year follow-up evaluation. Neurosurg Focus 2007;22:E7. [Crossref] [PubMed]
- Guehring T, Omlor GW, Lorenz H, et al. Disc distraction shows evidence of regenerative potential in degenerated intervertebral discs as evaluated by protein expression, magnetic resonance imaging, and messenger ribonucleic acid expression analysis. Spine (Phila Pa 1976) 2006;31:1658-65. [Crossref] [PubMed]
- Guehring T, Omlor GW, Lorenz H, et al. Stimulation of gene expression and loss of anular architecture caused by experimental disc degeneration--an in vivo animal study. Spine (Phila Pa 1976) 2005;30:2510-5. [Crossref] [PubMed]
- Guehring T, Unglaub F, Lorenz H, et al. Intradiscal pressure measurements in normal discs, compressed discs and compressed discs treated with axial posterior disc distraction: an experimental study on the rabbit lumbar spine model. Eur Spine J 2006;15:597-604. [Crossref] [PubMed]
- Senegas J. Surgery of the intervertebral ligaments, alternative to arthrodesis in the treatment of degenerative instabilities. Acta Orthop Belg 1991;57 Suppl 1:221-6. [PubMed]
- Sénégas J. Mechanical supplementation by non-rigid fixation in degenerative intervertebral lumbar segments: the Wallis system. Eur Spine J 2002;11 Suppl 2:S164-9. [PubMed]
- Talwar V, Lindsey DP, Fredrick A, et al. Insertion loads of the X STOP interspinous process distraction system designed to treat neurogenic intermittent claudication. Eur Spine J 2006;15:908-12. [Crossref] [PubMed]
- Villarejo F, Carceller F, de la Riva AG, et al. Experience with coflex interspinous implant. Acta Neurochir Suppl 2011;108:171-5. [Crossref] [PubMed]
- Samani J. Study of a Semi-Rigid Interspinous U Fixation System. Spinal Surgery, Child Orthopaedics 2002;1707.
- Maida G, Marcati E, Sarubbo S. Heterotopic ossification in vertebral interlaminar/interspinous instrumentation: report of a case. Case Rep Surg 2012;2012:970642.
- Tian NF, Wu AM, Wu LJ, et al. Incidence of heterotopic ossification after implantation of interspinous process devices. Neurosurg Focus 2013;35:E3. [Crossref] [PubMed]
- Parker SL, Anderson LH, Nelson T, et al. Cost-effectiveness of three treatment strategies for lumbar spinal stenosis: Conservative care, laminectomy, and the Superion interspinous spacer. Int J Spine Surg 2015;9:28. [Crossref] [PubMed]
- van den Akker-van Marle ME, Moojen WA, Arts MP, et al. Interspinous Process Devices versus Standard Conventional Surgical Decompression for Lumbar Spinal Stenosis: Cost Utility Analysis. Spine J 2014. [Epub ahead of print]. [Crossref] [PubMed]
- Burnett MG, Stein SC, Bartels RH. Cost-effectiveness of current treatment strategies for lumbar spinal stenosis: nonsurgical care, laminectomy, and X-STOP. J Neurosurg Spine 2010;13:39-46. [Crossref] [PubMed]